"These data provide support for implementation of intravenous thrombolysis in patients who fall within the full time window up to 9 hours since last known well or midpoint of sleep and who were eligible in the EXTEND trial," Dr. Bruce Campbell of Royal Melbourne Hospital and the University of Melbourne, in Parkville, Australia, and colleagues write in JAMA Neurology.
"Further trials will test whether intravenous thrombolysis can benefit patients with perfusion mismatch up to 24 hours after the time they were last known to be well," they add.
In an earlier meta-analysis of individual patient data from the EXTEND, ECASS4-EXTEND and EPITHET randomized trials, the researchers demonstrated overall benefit of intravenous alteplase given 4.5 to nine hours from symptom onset if perfusion mismatch was favorable (https://bit.ly/3oIQLEW). But about half of the patients had wake-up stroke, and so the number of patients treated after 4.5 to six hours and six to nine hours was relatively small.
To explore the consistency of the benefits of thrombolysis across different time windows, the team performed an analysis of functional outcomes by reperfusion status. Reperfusion was defined as more than 90% reduction in time to maximum of more than six seconds' lesion volume between baseline and 24-hour perfusion imaging in EXTEND and between baseline and day 3 imaging in EPITHET.
Among 270 patients with assessable reperfusion data (92%) from CT or MR scans, alteplase significantly boosted reperfusion relative to placebo (51% vs. 28%, P<0.001). There was no difference in median age or National Institutes of Health Stroke Scale scores between patients with and without reperfusion.
Patients with reperfusion had better functional outcomes as assessed at 90 days on the modified Rankin Scale by clinicians blinded to treatment allocation (common odds ratio, 7.7; P<0.001).
This was true in each of the three time windows - 4.5 to six hours, six to nine hours and wake-up stroke - and there was no association between time to randomization and the beneficial effect of reperfusion (P=0.63).
Likewise, there was no significant difference in rates of symptomatic hemorrhage, which ranged from 5.5% to 7.1%.
In an email to Reuters Health, Dr. Campbell emphasized that the results "do not mean we have any license to assess patients more slowly."
"The proportion of patients with favorable perfusion mismatch reduces over time so the faster you get patients to hospital and imaged, the more patients have salvageable brain tissue and will be eligible for thrombolysis," he said. "These data simply mean that some patients who are unavoidably delayed in reaching hospital and previously excluded from treatment may now benefit from thrombolysis if their brain imaging remains favorable."
He noted, "In Australia, we have month-by-month 'living' clinical-practice-guideline updates and we now recommend thrombolysis 4.5-9h after stroke onset (including 9h from the midpoint of sleep in patients with stroke discovered on waking) if perfusion imaging is favorable. This is yet to enter guidelines in USA and Europe."
While CT perfusion imaging is needed to determine eligibility, he said this "is implemented widely in Australia (not just in major academic teaching hospitals) and so this treatment is available across a large number of metropolitan and rural hospitals."
The two trials did not have commercial funding, although Boehringer Ingelheim provided the drug under investigation. Several of Dr. Campbell's coauthors report financial ties to the company, which sells alteplase under the brand name Actilyse in Australia.
By Frederik Joelving
SOURCE: https://bit.ly/34NOgsX JAMA Neurology, online November 2, 2020.
Posted on
Previous Article
« Novel nanobiologic trains immunity, curbs tumor growth in mice Next Article
Topical TYK2/JAK 1 inhibitor effective and tolerable in mild-to-moderate AD »
« Novel nanobiologic trains immunity, curbs tumor growth in mice Next Article
Topical TYK2/JAK 1 inhibitor effective and tolerable in mild-to-moderate AD »
Related Articles
February 14, 2022
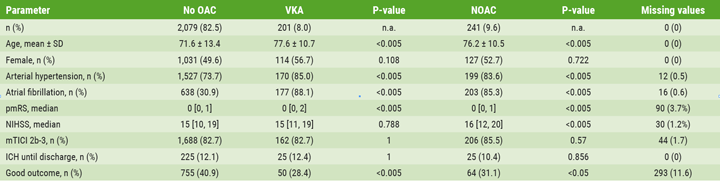
Clot-busting drugs appear safe in stroke patients taking blood thinners
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

