https://doi.org/10.55788/5fee6c07
The IL-23 inhibitor risankizumab was tested in participants with moderately to severely active UC with an inadequate response or intolerance to conventional and/or advanced therapies in a double-blind, placebo-controlled, phase 3 trial called INSPIRE (NCT03398148) [1]. Participants received 1,200 mg of risankizumab intravenously every 4 weeks (n=650) or a placebo (n=325). At baseline, about 35% of the participants were on corticosteroids, 73% were on aminosalicylates, and 16.5% were on immunosuppressants. Also, over 50% of the participants had an inadequate response or were intolerant to advanced therapies. The primary endpoint was the clinical remission rate at week 12, per adapted Mayo score, defined as stool frequency subscore ≤1 and not greater than baseline, rectal bleeding subscore of 0, and endoscopic subscore ≤1 without friability. Prof. Edouard Louis (Liège University Hospital, Belgium) presented the key results.
The primary endpoint was met by 20.3% of the participants in the risankizumab arm and by 6.2% of those in the placebo arm (P<0.0001). The corresponding clinical remission rates in the advanced therapies-naïve population were 29.7% and 8.4%. In those with an inadequate response or intolerance to advanced therapies, the clinical remission rates were 11.4% and 4.3%, respectively. Furthermore, the clinical response rate per adapted Mayo score at week 12 was 64.3% in the risankizumab arm and 35.7% in the placebo arm (P<0.0001). Notably, the clinical response rates already favoured risankizumab over placebo at week 4 (52.2% vs 30.5%; P<0.0001). Prof. Louis added that endoscopic, histologic, and patient-reported endpoints significantly favoured risankizumab over placebo.
Adverse events (AEs) were reported in 49.7% of the participants on placebo and 42.1% of those on risankizumab. Finally, the rate of serious AEs appeared to be higher in the placebo arm, at 10.2%, compared with 2.3% in the active arm. Worsening of UC (10.2%), anaemia (6.5%), and COVID-19 (5.9%) were the most common AEs in the placebo arm. In the risankizumab arm, the corresponding rates for these AEs were 1.7%, 3.4%, and 4.8%. Finally, hepatic events occurred numerically more frequently in the placebo arm than in the risankizumab arm (4.3% vs 1.5%).
Induction therapy with risankizumab showed benefits over placebo in clinical, endoscopic, histologic, and patient-reported outcomes in participants with UC, and was well-tolerated in this population.
- Louis E, et al. Risankizumab induction therapy in patients with moderately to severely active ulcerative colitis: efficacy and safety in the randomised phase 3 INSPIRE study. OP21, UEG Week 2023, 14–17 October, Copenhagen, Denmark.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« Risankizumab resolves extraintestinal manifestations in CD Next Article
Guselkumab provides benefits in UC regardless of advanced therapy history »
« Risankizumab resolves extraintestinal manifestations in CD Next Article
Guselkumab provides benefits in UC regardless of advanced therapy history »
Table of Contents: UEGW 2023
Featured articles
SEQUENCE: Risankizumab doubles endoscopic remission rates compared with ustekinumab in CD
What’s New in Artificial Intelligence
Digital intervention relieves symptoms and improves QoL in IBS
GastroGPT: Successful proof-of-concept study of gastroenterology-specific large language model
Other Therapeutics and Outcomes
Primary results from MAESTRO-NASH trial: resmetirom efficacious for NASH
Apraglutide: Advancing the treatment of short bowel syndrome
Endobiliary radiofrequency ablation in pCCA: a pilot study
Raising awareness for microscopic colitis: disease course and predictors
Outcomes of IBD Trials
DIVERSITY1: Filgotinib results in Crohn’s disease leave investigators puzzled
SEQUENCE: Risankizumab doubles endoscopic remission rates compared with ustekinumab in CD
Guselkumab provides benefits in UC regardless of advanced therapy history
INSPIRE: Risankizumab meets all efficacy endpoints in UC
Risankizumab resolves extraintestinal manifestations in CD
Obefazimod takes the spotlight as promising UC treatment
Rapid response to upadacitinib boosts outcomes in severe Crohn’s disease
LUCENT trials: Mirikizumab works in UC, regardless of targeted therapy history
ARTEMIS-UC: New kid in town for UC
Breakthroughs in Colorectal Lesions
Safer removal of large polyps with cold snare technique
Higher recurrence rates with cold snare EMR than with conventional EMR
How to deal with at-risk patients above the CRC screening age limit?
European CRC screening needs to be revised
Advances in Upper Endoscopy and Colonoscopy
Epinephrine boosts efficiency in gastric ESD
Artificial intelligence-aided colonoscopy did not improve outcomes in Lynch syndrome
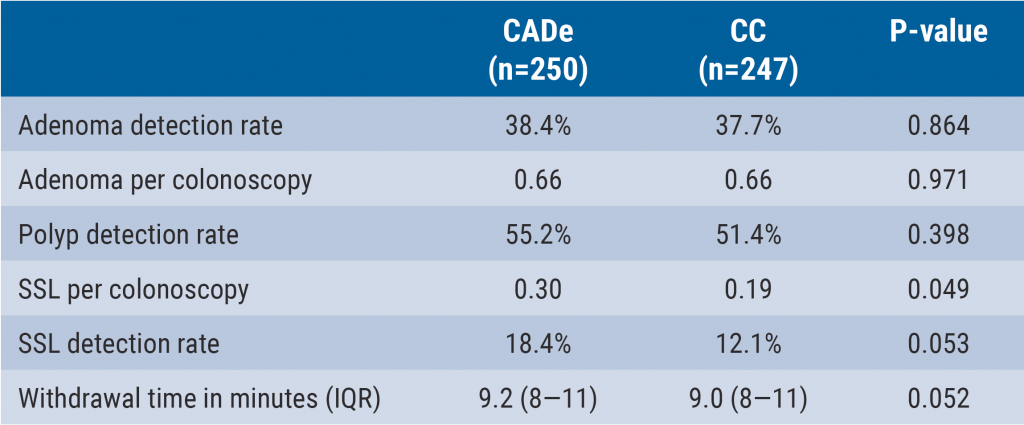
Can computer technology improve our everyday colonoscopy results?
Is AI-assisted colonoscopy ready for clinical practice?
Should we use E-SEMS or EVT for traumatic oesophageal perforations?
Related Articles
December 7, 2023
Can computer technology improve our everyday colonoscopy results?
December 7, 2023
Epinephrine boosts efficiency in gastric ESD
December 7, 2023
Is AI-assisted colonoscopy ready for clinical practice?
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

