https://doi.org/10.55788/8861a327
A large and unmet need exists for a more effective therapy in the management of HS. An interesting novel agent under investigation is the nanobody sonelokimab, a humanised antibody targeting IL-17A and IL-17F. Increasing evidence highlights IL-17A and IL-17F-mediated inflammation in HS pathogenesis. “Some patients go on to develop tunnels and draining fistulas. And we know that IL-17A and IL-17F are even higher in those with tunnels compared with patients that don’t develop tunnels,” Prof. Brian Kirby (St. Vincent´s University Hospital, Ireland) explained [1]. In addition, there is an albumin-binding domain. Due to its small molecular size and its ability to bind to albumin, sonelokimab is able to penetrate inflamed tissue which is otherwise difficult-to-treat; thus, directly targeting the site of inflammation.
Prof. Kirby presented the 12-week results of the double-blind, placebo-controlled, phase 2 MIRA trial (NCT05322473). This trial included adult patients with HS, Hurley stage II/III, a total abscess and/or inflammatory nodule count of ≥5, and the presence of HS lesions in ≥2 anatomical regions. They received either 120 mg or 240 mg sonelokimab, placebo, or adalimumab as an active comparator (to validate clinical findings but not powered for any statistical comparison). The primary study endpoint was the proportion of participants achieving a ≥75% reduction in total nodule counts from baseline with no new abscess or tunnel draining count (i.e. HiSCR 75).
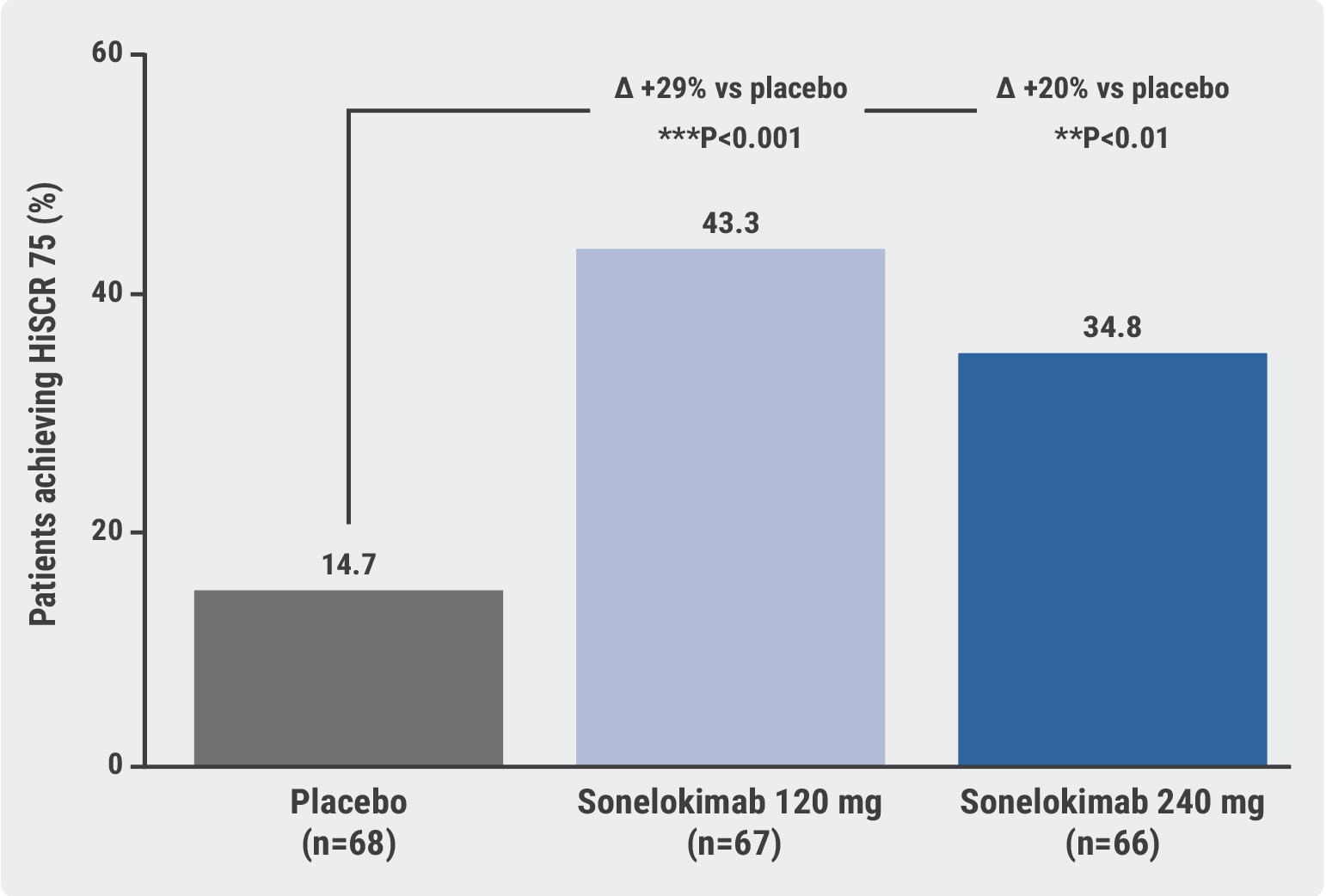
All in all, 234 participants could be included and >95% completed week 12. Significantly more participants treated with sonelokimab achieved the primary endpoint at week 12 compared with placebo (43.3% treated with 120 mg and 34.8% treated with 240 mg vs 14.7% in the placebo group; P<0.001 for the first and P<0.01 for the second comparison; see Figure).
Figure: Sonelokimab met the primary endpoint of HiSCR75 at week 12 [1]
“Sonelokimab works quickly. We see significant differences versus placebo as early as week 8,” Prof. Kirby said. Moreover, sonelokimab improved quality of life, as measured by the Dermatology Life Quality Index (DLQI; i.e. improvement of ≥4 points, which is considered clinically relevant) and led to less skin pain.
The nanobody was well tolerated in accordance with its known safety profile. Candida infections occurred more frequently in the sonelokimab groups (e.g. 6% cases of oral candidiasis in the low-dose group and 12.1% in the high-dose group compared with no cases in the placebo group) but were generally mild-to-moderate and did not lead to treatment withdrawal.
- Kirby B, et al. Efficacy and safety of the IL-17A- and IL-17F-inhibiting Nanobody® Sonelokimab in patients with active, moderate-to-severe hidradenitis suppurativa: Results from the global, randomized, double-blind, placebo-controlled phase 2 MIRA trial. D1T01.1H, EADV Congress 2023, 11–14 October, Berlin, Germany.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« Anti-IL17 blockade leads to maintained pain reduction in patients with HS Next Article
Skin tape stripping allows a novel precision medicine approach in HS »
« Anti-IL17 blockade leads to maintained pain reduction in patients with HS Next Article
Skin tape stripping allows a novel precision medicine approach in HS »
Table of Contents: EADV 2023
Featured articles
Tapinarof on course to become a new topical treatment in AD
AD and Eczema in 2023
Tapinarof on course to become a new topical treatment in AD
Upadacitinib provides sustained skin clearance in adolescents and adults with AD
Sustained deep clinical and itch responses with novel IL-13 inhibitor
IL-13 inhibitor shows potential in atopic dermatitis
Encouraging results for amlitelimab in atopic dermatitis
Chronic hand eczema: patients share similar molecular signatures regardless of AD status
Severe hand eczema: dupilumab could be a future treatment
Psoriasis News
Dual IL-17 blockade yields efficacy on joints and skin
High-dose subcutaneous spesolimab prevents GPP flares up to week 48
Drug survival of guselkumab and risankizumab seems superior to other biologics
IL-23 blockers may lower the risk of developing inflammatory and psoriatic arthritis
First-in-class oral IL-23 inhibitor safe and effective for moderate-to-severe plaque psoriasis
Hidradenitis Suppurativa: End of the Diagnostic and Therapeutic Draught
Skin tape stripping allows a novel precision medicine approach in HS
Nanobodies: A novel way to treat HS
Anti-IL17 blockade leads to maintained pain reduction in patients with HS
Vitiligo: Novel Treatment Options
JAK1 inhibition: a promising forthcoming treatment option in vitiligo
Vitiligo: Continuation of topical ruxolitinib successful in many initial non-responders
Alopecia Areata: Novel Developments
JAK3/TEC inhibition achieves clinically meaningful responses in AA
Alopecia areata: remarkable regrowth rates with deuruxolitinib
Botanical drug solution improves hair regrowth in children and adolescents with AA
What’s New in Other Disease Entities
Nemolizumab shows high success rates in prurigo nodularis
Remibrutinib reduces itch, sleep problems, and activity impairment in patients with CSU
Innovative wound gel reduces frequency of painful dressing changes in epidermolysis bullosa
Best of the Posters
Women with psoriasis face increased adverse effects with systemic therapy
Improved AI tool shows high sensitivity rates in skin cancer detection
Dermoscopy training combined with AI significantly improves skin cancer detection
Related Articles
November 19, 2021
Updated results of SECOMBIT trial
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

