https://doi.org/10.55788/b2bc155a
The risk for melanoma is affected by hereditary factors (5%), DNA replication errors (9%), but mostly environmental factors (86%), such as UV radiation. In addition, important clinical risk factors for developing sporadic melanoma are a history of skin cancer, having ≥100 naevi, ≥ 5 atypical naevi, and red hair (see Figure).
Figure: Clinical risk factors of sporadic melanoma [1]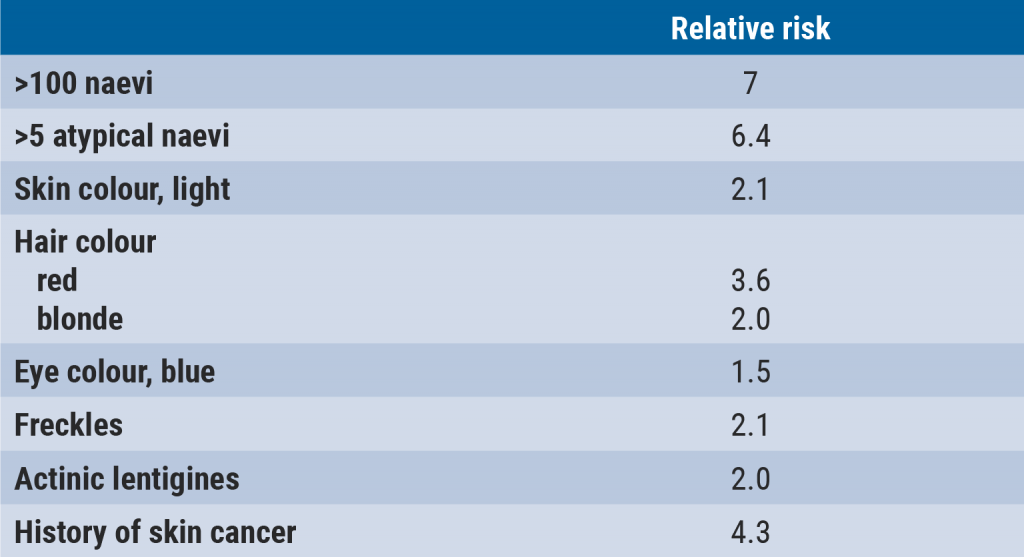
Individuals with ≥100 naevi or ≥5 atypical naevi are eligible for screening in the Netherlands. This screening includes a total body inspection, once a year, ideally with total body photography, applying dermatoscopy on suspected naevi and providing advice on self-inspection of the skin and sunbathing. “10,000 to 100,000 individuals in the Netherlands fulfil these criteria, but not all of them are screened regularly,” said Dr van Doorn. In addition, a study followed 1,100 individuals who fitted the screening criteria and were screened for 5 consecutive years. The incidence of melanoma was 1.1% per surveillance year. Most melanomas were discovered by the dermatologist (78%), whereas the patients detected 17% of their melanoma.
“Another group that we screen are children with congenital naevi,” continued Dr van Doorn. The screening and frequency of screening are based on the ‘projected adult size’ of these naevi, the number of congenital naevi, and whether there are satellites present. Then there is the group of individuals with hereditary melanoma, which comprises approximately 10% of all melanoma. The eligibility criterium for this screening is 3 melanoma within the family in at least 2 different first-degree family members.
Dr van Doorn added that individuals with CDKN2A mutations are at higher risk for melanoma, as well as for pancreas carcinoma and head/neck tumours. Similarly, those with BAP1-associated tumour predisposition syndrome have an increased risk for melanoma and several other tumours. “Patients with these kinds of mutations or other rare mutations need to receive a much broader screening, based on their gene deficiency,” clarified Dr van Doorn. “A clinical genetical consultation will further inform the patient on screening options, DNA testing, and advice for other family members. For example, first-degree and second-degree relatives of patients who carry CDKN2A or BAP1 mutations should be screened for melanoma and other cancers.
Follow-up
“Once we detect a melanoma in the screened population, we follow the patient based on the AJCC classification,” explained Dr van Doorn. “There is, however, no clear consensus on the frequency of follow-up.” He explained that the Leiden University Medical Center follows the follow-up protocol of the MELFO study [2]. This study showed that stage I–II patients with pT1b-pT2a tumours only need to be screened once a year, those with pT2b-pT3a tumours can be safely monitored with 2 screening per year in the first 2 years and yearly screenings in the subsequent 3 years, and that patients with pT3b-pT4b tumours should receive 3 screenings per year in the first 2 years, 2 screenings per year in the third year, and yearly screenings in the following 2 years. Furthermore, patients with stage III melanoma will primarily be followed by the surgeon but will receive yearly screenings by a dermatologist. Finally, patients with stage IV melanoma will primarily be followed by the oncologist and receive yearly screenings by a dermatologist.
“Although I have outlined the current state of affairs with regard to the surveillance and follow-up of patients with melanoma, it is still not completely established which of the 10,000 to 100,000 patients with multiple atypical naevi in the Netherlands should be screened and how frequently we should provide follow-up visitations for our patients with melanoma,” concluded Dr van Doorn.
- Van Doorn R. Follow-up na BCC, SCC en melanoom: te veel of te weinig? Blok 2, Dermatologendagen 2023, 9–10 March, Ermelo, the Netherlands.
- Deckers EA, et al. Ann Surg Oncol. 2020;27(5):1407–1417.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« When to screen for anal intraepithelial neoplasia? Next Article
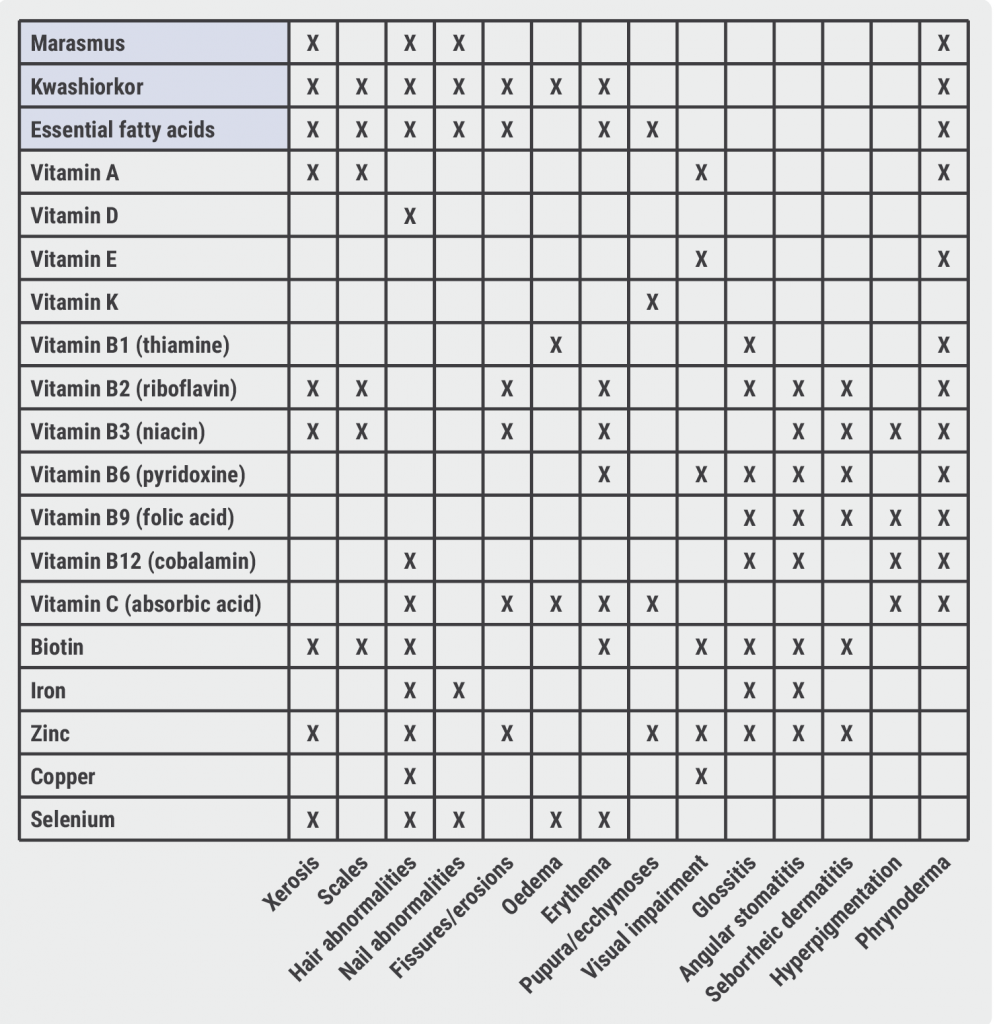
Skin diseases and nutrition »
« When to screen for anal intraepithelial neoplasia? Next Article
Skin diseases and nutrition »
Table of Contents: DDD 2023
Featured articles
Dermato-Oncology
The role of surgeons in stage I–II melanoma
Melanoma: Surveillance and follow-up
When to screen for anal intraepithelial neoplasia?
JAK Inhibitors
Eligibility and selection of JAK inhibitors for constitutional eczema
Nutrition and the Skin
Obesity and the skin: state of affairs
What's New?
The importance of anti-microbial proteins in the skin
OCT non-inferior to biopsy in basal cell carcinoma
Infections
Scabies: Therapy failure and tips for the clinic
Related Articles
May 10, 2023
OCT non-inferior to biopsy in basal cell carcinoma
May 10, 2023
Skin diseases and nutrition
May 10, 2023
The role of surgeons in stage I–II melanoma
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

