https://doi.org/10.55788/61d94762
The treatment for scabies
According to the current IUSTI guidelines, the standard therapies to treat scabies are permethrin 5% cream (can be repeated once after 7–14 days), oral ivermectin 200 μg/kg (repeat after 7 days), or benzyl benzoate lotion 10–25% (on days 1,2 and repeat after 7 days) [2]. Dr Vodegel added that this last treatment is mostly for pregnant patients and that the second treatment with ivermectin should preferably be administered within 7 to 10 days; a waiting period of 14 days is arguably too long when the lifespan of the mite is considered.
“Also, topical treatments need to be applied to all skin regions at night and left in place for 8–12 hours. The most frequently missed skin areas are the ankles, the hamstrings, toes and feet, the nails, and the armpits,” explained Dr Vodegel. Therefore, it is important to inform the patient that the nails need to be clipped before applying topical treatments, the hands need to be re-treated after washing the hands, and other members of the household need to be treated simultaneously, including babies. Then there are hygienic measurements that need to be taken, such as washing, dry cleaning, and sealing clothes. Dr Vodegel stressed that the current IUSTI guideline did not offer recommendations on the treatment of persons who were in close contact with the patient. “This could be a major reason for therapy failure,” he said.
Therapy failure or resistance
According to Dr Vodegel, causes of therapy failure include:
- a wrong diagnosis,
- local skin reactions because of the applied cream,
- hypersensitivity reaction,
- not strictly following hygiene protocol,
- not treating relatives and other contacts,
- non-compliance to therapy, and
- possibly therapy resistance.
“It is still unclear whether therapy resistance is a real issue, or that infections persist because patients did not follow the hygienic measurements strictly,” added Dr Vodegel. “Perhaps the information we provide to our patients is more important than actual therapy resistance.” If a therapy is not effective, the options are to repeat the current therapy, switch to another therapy, or combine ivermectin with permethrin. It must be noted that patients should not eat 2 hours before or after taking ivermectin. Furthermore, the scalp should be treated in children younger than 12 years, fragile elderly patients, and other vulnerable groups if they receive a permethrin treatment.
Future directions
Dr Vodegel ended his presentation by proposing actions that may counter the rising incidence of scabies in the Netherlands. According to Dr Vodegel, the Dutch guideline for the management of scabies is being revised at the moment and the concept version of the chapter related to the treatment has already been completed. This update includes recommendations on treating symptom-free relatives and other contacts, and renewed advice concerning the second treatment with permethrin. “It is important to recognise that the policy and possibilities with respect to managing scabies vary between regions. Also, educating general practitioners and developing a protocol for scabies outbreaks in institutions such as nursing homes and daycare centres would be improvements to our current management of scabies. Finally, we need prospective studies to gain more insight into why therapies fail in patients with scabies,” concluded Dr Vodegel.
- Vodegel RM. Scabies. Blok 1, Dermatologendagen 2023, 9–10 March, Ermelo, the Netherlands.
- Salavastru CM, et al. J Eur Acad Dermatol Venereol. 2017;31(8):1248–1253.
Posted on
Previous Article
« Life-threatening skin infections Next Article
The importance of anti-microbial proteins in the skin »
« Life-threatening skin infections Next Article
The importance of anti-microbial proteins in the skin »
Table of Contents: DDD 2023
Featured articles
Dermato-Oncology
The role of surgeons in stage I–II melanoma
Melanoma: Surveillance and follow-up
When to screen for anal intraepithelial neoplasia?
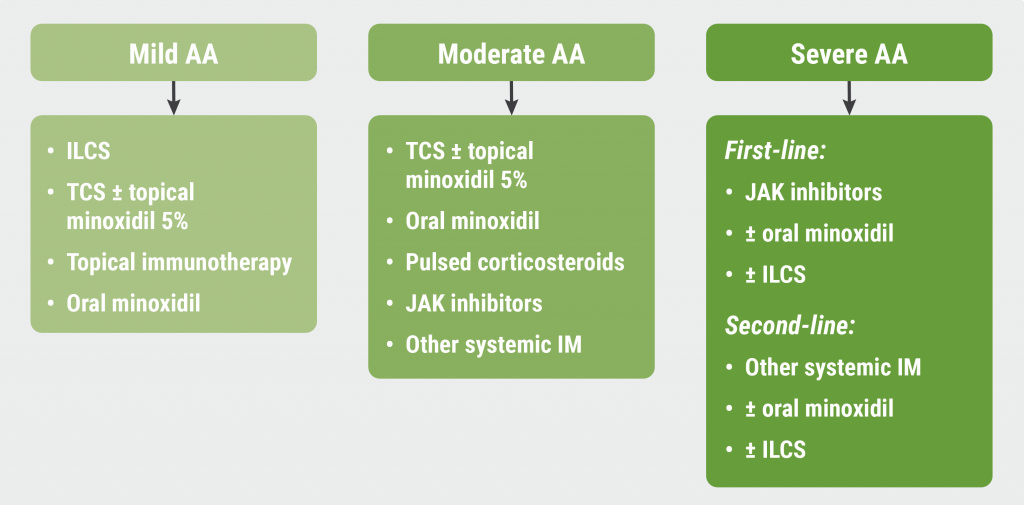
JAK Inhibitors
Eligibility and selection of JAK inhibitors for constitutional eczema
Nutrition and the Skin
Obesity and the skin: state of affairs
What's New?
The importance of anti-microbial proteins in the skin
OCT non-inferior to biopsy in basal cell carcinoma
Infections
Scabies: Therapy failure and tips for the clinic
Related Articles
May 10, 2023
The rise of JAK inhibitors for alopecia areata
May 10, 2023
Scabies: Therapy failure and tips for the clinic
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

