https://doi.org/10.55788/7bdf0504
The usual suspects
Streptococcus pyogenes A and Staphylococcus aureus are the usual suspects for skin infections. Since these bacteria are sensitive to antibiotics, infections with these pathogens are usually easy to treat. Yet, in some cases, infections with one of these bacteria can lead to life-threatening situations.
“Impetigo and erysipelas rarely lead to haemodynamic issues,” continued Dr Arend. “The same is true for folliculitis. However, if a folliculitis turns into a boil, haematogenic spread may occur, especially if the boil is manipulated by the patient.” Special attention needs to be given to a boil on the tip of the nose. If this infection spreads to the sinus cavernosus, the mortality rate is high. “The skin of the tip of the nose has a venous connection to the sinus cavernosus and the risk of spreading is, therefore, profound,” added Dr Arend.
Then there is cellulitis, which will usually not lead to severe complications or life-threating situations, according to Dr Arend. “The first potentially life-threatening skin infection I would like to discuss is necrotising cellulitis,” said Dr Arend. This condition often arises from a combined infection with anaerobic bacteria and gram-negative streptococcus pyogenes in patients with vascular diseases or diabetes. However, a mono-infection with streptococcus pyogenes may also lead to necrotising cellulitis. It can easily spread through the vascular system, leading to sepsis.
Finally, there is necrotising fasciitis, often involving the same pathogens as those that cause necrotising cellulitis. Necrotising fasciitis is characterised by excruciating pain and high fever. “Discriminating between these 2 life-threatening skin infections is relevant because immediate surgery is necessary to prevent further deterioration of the fascia in case of necrotising fasciitis. Dermatologists should pay attention to the absence of capillary refill, purple, brown, bronze, or white discolourations, loss of sensibility, crepitations, and bullae, which are symptoms of necrotising skin infections.”
Unusual suspects
Dr Arend also discussed some unusual pathogens that may lead to severe skin infections. She mentioned that an infection with capnocytophaga canimorsus may lead to necrotising fasciitis. “Severe cases may arise after a dog bite in a patient with immunosuppression,” said Dr Arend. Similarly, pasteurella multocida infections, which are caused by a cat bite, could lead to necrotising fasciitis. Another unusual suspect for the development of necrotising fasciitis is vibrio vulnificus. Working with oysters is a risk factor for infection.
Toxin-mediated diseases
Dr Arend also highlighted 3 toxin-mediated diseases that may lead to life-threatening skin infections. Staphylococcus-scalded skin syndrome is seen in small children with, for example, an infected nail. The exfoliating toxin may spread systemically. “Fortunately, the expansion is usually superficial, and the mortality rate is ‘only’ 5%,” mentioned Dr Arend. If this syndrome occurs in adults, which is uncommon, the mortality rate is 50%.
Another toxin-mediated disease is scarlet fever. It usually starts with a throat infection and typical clinical signs of this condition are the so-called ‘strawberry tongue’ and the rash-free zone around the mouth and nose. “The scarlet rash that individuals with this disease develop is toxin-mediated,” clarified Dr Arend.
Finally, toxic shock syndrome is life-threatening if it is caused by streptococcus pyogenes, whereas an underlying infection with staphylococcus aureus mostly leads to a less severe disease course.
Dr Arend also named some life-threatening infections with clear skin manifestations that dermatologists should be aware of. These include meningococcal sepsis, staphylococcal sepsis, endocarditis, typhoid fever, and viral haemorrhagic fever. Her last remark to the audience was not to forget to consider atypical mycobacteria in immunosuppressed patients.
- Arend S. Levensbedreigende huidinfecties. Blok 1, Dermatologendagen 2023, 9–10 March, Ermelo, the Netherlands.
Posted on
Previous Article
« OCT non-inferior to biopsy in basal cell carcinoma Next Article
Scabies: Therapy failure and tips for the clinic »
« OCT non-inferior to biopsy in basal cell carcinoma Next Article
Scabies: Therapy failure and tips for the clinic »
Table of Contents: DDD 2023
Featured articles
Dermato-Oncology
The role of surgeons in stage I–II melanoma
Melanoma: Surveillance and follow-up
When to screen for anal intraepithelial neoplasia?
JAK Inhibitors
Eligibility and selection of JAK inhibitors for constitutional eczema
Nutrition and the Skin
Obesity and the skin: state of affairs
What's New?
The importance of anti-microbial proteins in the skin
OCT non-inferior to biopsy in basal cell carcinoma
Infections
Scabies: Therapy failure and tips for the clinic
Related Articles
May 10, 2023
The role of surgeons in stage I–II melanoma
May 10, 2023
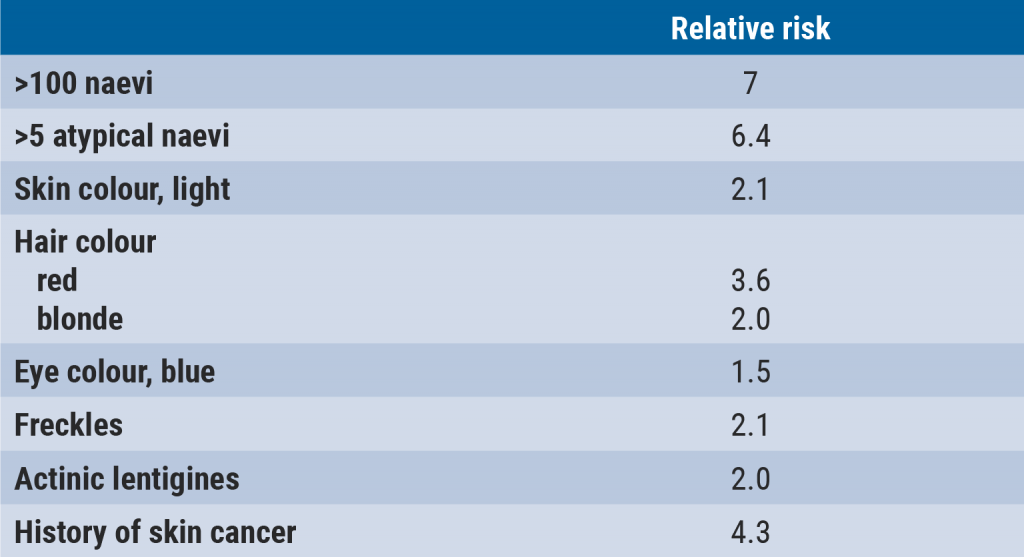
Melanoma: Surveillance and follow-up
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

