https://doi.org/10.55788/2ddcf9dc
While MRAs are well-established in reducing hospitalisations and mortality in HF with reduced ejection fraction (HFrEF), their benefits in HF with mildly reduced (HFmrEF) or preserved ejection fraction (HFpEF) have been less clear. Prof. Pardeep Jhund (University of Glasgow, Scotland) presented a meta-analysis on this topic, which was simultaneously published in The Lancet. The analysis pooled data from 4 major trials: RALES and EMPHASIS-HF, which focused on HFrEF, and TOPCAT and FINEARTS-HF, which focused on HFmrEF and HFpEF [1–5].
The meta-analysis included 13,846 patients and revealed that MRAs significantly reduced the risk of cardiovascular death or HF hospitalisation versus placebo, with a hazard ratio (HR) of 0.77 (95% CI 0.72–0.83; P<0.001). However, the efficacy varied significantly between the HF subtypes. In patients with HFrEF, MRAs showed greater benefit, reducing the risk by 34% (HR 0.66; 95% CI 0.59–0.73; P<0.001). In contrast, the reduction was more modest in patients with HFmrEF or HFpEF, with a 13% risk reduction (HR 0.87; 95% CI 0.79–0.95; P=0.004).
The analysis also found that MRAs significantly decreased HF hospitalisations as an individual component in both HFrEF (HR 0.63; 95% CI 0.55–0.72; P<0.001) and HFmrEF/HFpEF (HR 0.82; 95% CI 0.74–0.91; P<0.001) populations. Cardiovascular death was reduced in patients with HFrEF (HR 0.72; 95% CI 0.63–0.82; P<0.001) but not in those with HFmrEF or HFpEF (HR 0.92; 95% CI 0.80–1.05; P=0.20). Similarly, all-cause mortality was reduced in HFrEF (HR 0.73; 95% CI 0.65–0.83; P<0.001) but not in patients with HFmrEF or HFpEF (HR 0.94; 95% CI 0.85–1.03; P=0.19).
In terms of safety, the use of MRAs was associated with a doubled risk of hyperkalaemia compared with placebo (OR 2.27; 95% CI 2.02–2.56; P<0.001), though the incidence of severe hyperkalaemia (serum potassium >6.0 mmol/L) remained low at 2.9% versus 1.4%, and there were no deaths due to hyperkalaemia. In line with this, MRAs reduced the risk of hypokalaemia by half (OR 0.51; 95% CI 0.45–0.57; P<0.001).
These findings suggest that MRAs reduce cardiovascular death and hospitalisations across the spectrum of EF. It remains to be investigated whether differences between newer generations of non-steroidal MRAs that have differential effects in cardiac and kidney tissue and different tolerability than traditional steroidal MRAs explain positive findings in FINEARTS-HF relative to other trials. This new meta-analysis reinforces the need for tailored treatment approaches depending on the type of HF and ejection fraction at the individual level.
Relevant readings:
- FINEARTS-HF: Finerenone improves outcomes in heart failure with preserved ejection fraction (ESC 2024)
- Application of guideline-directed medical therapy in patients with HFrEF in the Netherlands (HFA 2024)
- Antagonising the mineralocorticoid receptor beneficial for patients with diabetes and CKD (ESC 2021)
- Finerenone reduces the risk of AF onset in patients with CKD and diabetes (ACC 2021)
- Jhund P, et al. MRAs in heart failure – An individual patient data meta-analysis of randomised trials. HOTLINE 7, ESC Congress 2024, 30 Aug–02 Sept, London, UK.
- Jhund P, et al. Lancet 2024;404(10458):1119-1131.
- Pitt B, et al. N Engl J Med 1999;341(10):709-17.
- Zannad F, et al. N Engl J Med 2011;364(1):11-21.
- Pitt B, et al. N Engl J Med 2014;370(15):1383-92.
- Solommn S, et al. N Engl J Med 2024;391:1475-1485.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« MATTERHORN: Transcatheter repair matches surgery for HF with secondary mitral regurgitation Next Article
FINEARTS-HF: Finerenone improves outcomes in heart failure with preserved ejection fraction »
« MATTERHORN: Transcatheter repair matches surgery for HF with secondary mitral regurgitation Next Article
FINEARTS-HF: Finerenone improves outcomes in heart failure with preserved ejection fraction »
Table of Contents: ESC 2024
Featured articles
Meet the Expert: Dr Abdullahi Mohamed on Iron Deficiency in Patients with HF
2024 ESC Guidelines in a Nutshell
Guidelines for the management of elevated blood pressure and hypertension
Guidelines for the management of chronic coronary syndromes
Guidelines for the management of atrial fibrillation
Guidelines for the management of peripheral artery and aortic diseases
Crossing Borders in Arrhythmia
EPIC-CAD: What is the best antithrombotic approach in high-risk AF plus stable CAD?
OCEANIC-AF: Asundexian inferior to apixaban for ischaemic stroke prevention in AF
MIRACLE-AF: Elegant solution to improve AF care in rural China
SUPPRESS-AF: What is the value of adding LVA ablation to PVI in AF?
Clever Ideas for Coronary Artery Disease
ABYSS: Can beta-blocker safely be interrupted post-MI?
SWEDEGRAFT: Can a no-touch vein harvesting technique improve outcomes in CABG?
Bioadaptor meets expectations in reducing target lesion failures in coronary artery disease
REC-CAGEFREE I: Can we avoid permanent stenting with drug-coated balloons?
OCCUPI: OCT-guided PCI improves outcomes in complex CAD
Highway to Hypertension Control
Low-dose 3-drug pill GMRx2 shows promise in lowering BP
Is administering BP medication in the evening better than in the morning?
VERONICA: Improving BP control in Africa with a simple strategy
High-end Trials in Heart Failure
FINEARTS-HF: Finerenone improves outcomes in heart failure with preserved ejection fraction
MRAs show varied efficacy in heart failure across ejection fractions
MATTERHORN: Transcatheter repair matches surgery for HF with secondary mitral regurgitation
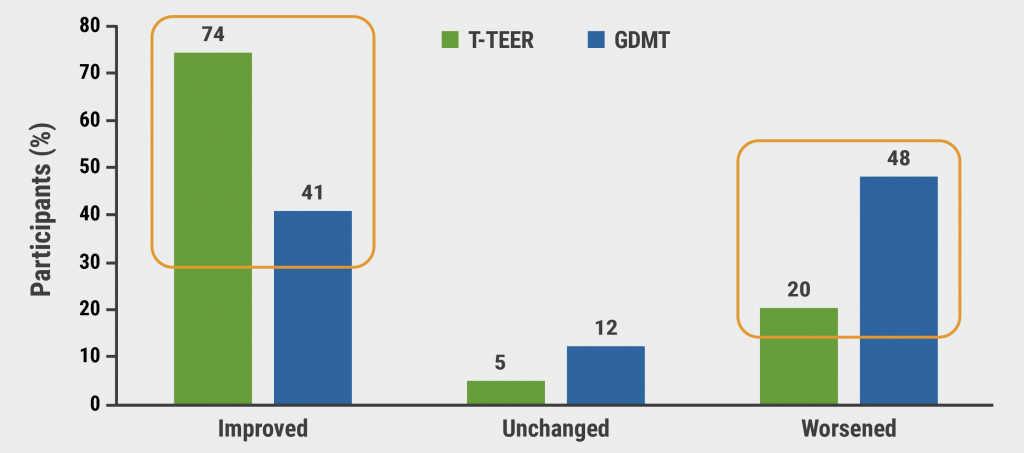
RESHAPE-HF2: Not a “tie-breaker” for TEER in heart failure
Practical Gains in Screening and Diagnostics
STEEER-AF: Shockingly low adherence to ESC atrial fibrillation guidelines
SCOFF: To fast or not to fast, that’s the question
WESTCOR-POC: Point-of-care hs-troponin testing increases emergency department efficiency
PROTEUS: Can AI improve decision-making around stress echocardiography?
RAPIDxAI: Can AI-augmented chest pain assessment improve cardiovascular outcomes?
Miscellaneous Achievements in Cardiology
HELIOS-B: Vutrisiran candidate for SoC in ATTR cardiomyopathy
Does RAS inhibitor discontinuation affect outcomes after non-cardiac surgery?
Novel approach to managing severe tricuspid regurgitation proves its value
NOTION-3: TAVI plus PCI improves outcomes in CAD plus severe aortic stenosis
RHEIA: TAVI outperformed surgery in women with aortic stenosis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com