https://doi.org/10.55788/84d0167b
“Choosing the optimal antithrombotic therapy for patients with CAD and AF is challenging,” expressed Dr Gi-Byoung Nam (Ulsan University Hospital, South Korea) [1]. “Patients with AF need prevention of thromboembolic events with anticoagulants and patients with CAD need antiplatelet therapy to prevent ischaemic events.” The combined use of these drugs comes with an increased risk of bleeding [2]. The authors of the current study hypothesised that edoxaban monotherapy would be superior to dual antithrombotic therapy in terms of a combined ischaemic and bleeding endpoint in patients with CAD and AF [1,3].
In the phase 4 EPIC-CAD trial (NCT03718559), 1,038 participants with high-risk AF and stable CAD from 18 sites in South Korea were randomised 1:1 to edoxaban monotherapy or to dual antithrombotic therapy with edoxaban plus a single anti-platelet agent. Stable CAD was defined as revascularisation for a chronic coronary syndrome at least 6 months prior, revascularisation for ACS at least 12 months prior, or anatomically confirmed coronary disease managed without revascularisation. The primary endpoint was a composite of all-cause death, stroke, systemic embolic events, myocardial infarction, unplanned urgent revascularisation, major bleeding, and clinically relevant non-major bleeding after 1 year of therapy.
Dual antithrombotic therapy led to more adverse events than edoxaban monotherapy, as revealed by the primary outcome (16.2% vs 6.8%; HR 0.44; 95% CI 0.30–0.65; P<0.001). The incidence of major ischaemic events was low in both of the 2 study arms (1.8% vs 1.6%; HR 1.23; 95% CI 0.48–3.10), whereas major or clinically relevant non-major bleeding was more common in the dual antithrombotic therapy arm than in the monotherapy arm (14.2% vs 4.7%; HR 0.34; 95% CI 0.22−0.53). Dr Nam acknowledged that the trial was underpowered for ischaemic thrombotic events as a sole endpoint.
The EPIC-CAD study suggests that edoxaban monotherapy is linked to a lower risk of bleeding compared with dual antithrombotic therapy with edoxaban and an antiplatelet agent in patients with AF and stable CAD. “The effect appeared to be driven by a decreased risk for bleeding events in the monotherapy arm,” concluded Dr Nam.
- Nam G-B, et al. Edoxaban-based long-term antithrombotic therapy for atrial fibrillation and stable coronary disease: The EPIC-CAD randomised clinical trial. HOTLINE 6, ESC Congress 2024, 30 Aug–02 Sept, London, UK.
- Gibson CM, et al. N Engl J Med 2016;375:2423.
- Cho MS, et al. N Engl J Med 2024; 1 Sept. DOI: 10.1056/NEJMoa2407362.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« OCEANIC-AF: Asundexian inferior to apixaban for ischaemic stroke prevention in AF Next Article
Guidelines for the management of peripheral artery and aortic diseases »
« OCEANIC-AF: Asundexian inferior to apixaban for ischaemic stroke prevention in AF Next Article
Guidelines for the management of peripheral artery and aortic diseases »
Table of Contents: ESC 2024
Featured articles
Meet the Expert: Dr Abdullahi Mohamed on Iron Deficiency in Patients with HF
2024 ESC Guidelines in a Nutshell
Guidelines for the management of elevated blood pressure and hypertension
Guidelines for the management of chronic coronary syndromes
Guidelines for the management of atrial fibrillation
Guidelines for the management of peripheral artery and aortic diseases
Crossing Borders in Arrhythmia
EPIC-CAD: What is the best antithrombotic approach in high-risk AF plus stable CAD?
OCEANIC-AF: Asundexian inferior to apixaban for ischaemic stroke prevention in AF
MIRACLE-AF: Elegant solution to improve AF care in rural China
SUPPRESS-AF: What is the value of adding LVA ablation to PVI in AF?
Clever Ideas for Coronary Artery Disease
ABYSS: Can beta-blocker safely be interrupted post-MI?
SWEDEGRAFT: Can a no-touch vein harvesting technique improve outcomes in CABG?
Bioadaptor meets expectations in reducing target lesion failures in coronary artery disease
REC-CAGEFREE I: Can we avoid permanent stenting with drug-coated balloons?
OCCUPI: OCT-guided PCI improves outcomes in complex CAD
Highway to Hypertension Control
Low-dose 3-drug pill GMRx2 shows promise in lowering BP
Is administering BP medication in the evening better than in the morning?
VERONICA: Improving BP control in Africa with a simple strategy
High-end Trials in Heart Failure
FINEARTS-HF: Finerenone improves outcomes in heart failure with preserved ejection fraction
MRAs show varied efficacy in heart failure across ejection fractions
MATTERHORN: Transcatheter repair matches surgery for HF with secondary mitral regurgitation
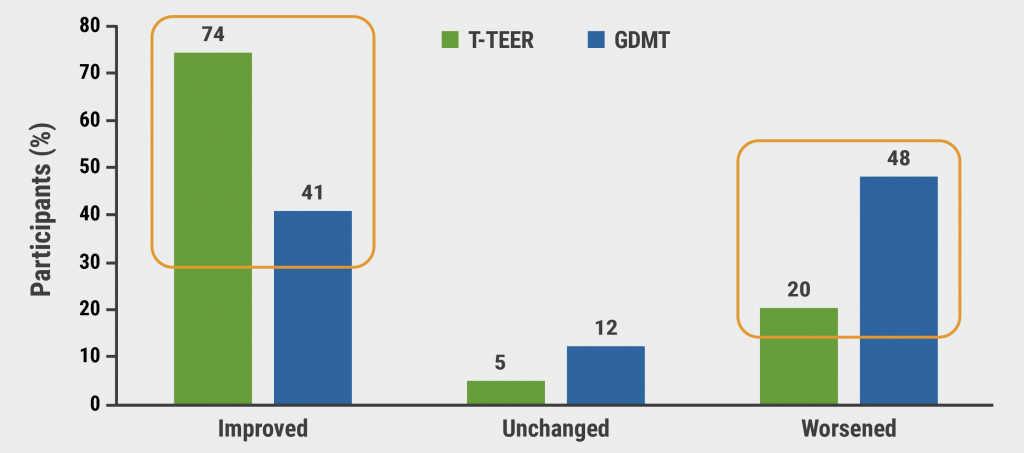
RESHAPE-HF2: Not a “tie-breaker” for TEER in heart failure
Practical Gains in Screening and Diagnostics
STEEER-AF: Shockingly low adherence to ESC atrial fibrillation guidelines
SCOFF: To fast or not to fast, that’s the question
WESTCOR-POC: Point-of-care hs-troponin testing increases emergency department efficiency
PROTEUS: Can AI improve decision-making around stress echocardiography?
RAPIDxAI: Can AI-augmented chest pain assessment improve cardiovascular outcomes?
Miscellaneous Achievements in Cardiology
HELIOS-B: Vutrisiran candidate for SoC in ATTR cardiomyopathy
Does RAS inhibitor discontinuation affect outcomes after non-cardiac surgery?
Novel approach to managing severe tricuspid regurgitation proves its value
NOTION-3: TAVI plus PCI improves outcomes in CAD plus severe aortic stenosis
RHEIA: TAVI outperformed surgery in women with aortic stenosis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com