Dr Steven Lubitz (Massachusetts General Hospital, MA, USA) explained that early detection of AF may prevent morbidity of this condition [1]. Since smartwatches and fitness trackers are often equipped with optical PPG sensors, software algorithms that analyse PPG data can detect AF on these wearable devices. Dr Lubitz and colleagues developed a software algorithm with overlapping PPG pulse tachogram sampling and assessed its positive predictive value for undiagnosed AF in various wearable Fitbit devices.
Participants of the Fitbit Heart Study (NCT04380415) were 22 years or older, possessed a compatible Fitbit device, and did not have a known AF diagnosis. The software reported an irregular heart rhythm detection (IHRD) if the algorithm registered ≥30 minutes of irregular rhythm. Patients with an IHRD received an ECG patch to wear for 1 week. In total, 455,669 participants enrolled in the study (median age 47 years, 71% women), of whom 4,278 (1%) received an IHRD notification. Of these participants, 1,057 (24.7%) completed the 1-week ECG patch period, illustrating the limited engagement of participants in this remote clinical trial. The primary endpoint was the positive predictive value of the first IHRD for AF during ECG monitoring.
The percentage of participants receiving an IHRD was higher among men and participants ≥65 years old. The positive predictive value of IHRD for AF was 98% and similar in the predefined age and sex subgroups. IHRD showed a sensitivity of 68% for AF measurement during ECG monitoring. In addition, participants who had an IHRD notification and completed ECG patch monitoring displayed AF in 32% of the cases. This percentage was equally divided across sex and age categories. Dr Lubitz added that the ≥65 years subgroup is an important category to consider since AF in these patients is associated with an increased risk of stroke.
Dr Gregory Marcus (University of California, CA, USA) presented another study on the remote management of AF [2,3]. He argued that the risk factors for AF, such as hypertension, age, male sex, and coronary disease, are mostly chronic and immutable, and that the acute triggers of AF are less well documented. Thus, the I-STOP-Afib trial (NCT03323099) aimed to test individual AF triggers using an innovative N-of-1 study design. Eligible adult participants were randomised to a data-tracking control group (n=248) or an experimental arm (n=251) and received a KardiaMobile to track AF episodes. Participants in the experimental arm could select a presumed trigger from a menu of triggers or add a customised trigger. These participants received instructions on when to avoid or expose themselves to the selected trigger during a 6-week period. Hereafter, they received individual (N-of-1) results of the enhanced risk of AF via exposure to the selected trigger. Subsequently, participants followed a 4-week lifestyle-changing period, in which they could adjust their behaviour in response to the results. The primary outcome was the change in the Atrial Fibrillation Effect on QualiTy-of-Life (AFEQT) questionnaire in the intention-to-treat population after 10 weeks. The most commonly selected triggers were caffeine (n=53), alcohol (n=43), reduced sleep (n=31), and exercise (n=30).
The average improvement on the AFEQT in the trigger-testing arm (+1.7) was not significantly larger than the average improvement in the control arm (+0.5; P=0.17). However, patients in the experimental arm documented 40% fewer self-reported AF episodes during the 4-week lifestyle-changing period compared with patients in the control arm (P<0.0001). This effect was driven by participants who selected alcohol, dehydration, or exercise as triggers. Per-protocol analysis of the N-of-1 trials displayed significant near-term effects of alcohol exposure on AF (OR 1.77) and customised triggers on AF (OR 4.09).
Discussant Dr Mina Chung (Cleveland Clinic, OH, USA) argued that conventional randomised controlled trials deliver average results for a pre-defined population, whereas the current N-of-1 study design has the potential to address individual patients. Although subgroup analyses in standard randomised controlled trials offer stratification of the results, the N-of-1 approach promises to surpass their ability to provide a truly personalised approach. According to Dr Chung, the significant secondary outcomes of the current study support the value of N-of-1 studies for individual patients.
- Lubitz SA, et al. Detection of Atrial Fibrillation in a Large Population using Wearable Devices: the Fitbit Heart Study. LBS04, AHA Scientific Sessions 2021, 13–15 November.
- Marcus GM, et al. The Individualized Studies of Triggers of Paroxysmal Atrial Fibrillation Trial. LBS04, AHA 2021 Scientific Sessions, 13–15 November.
- Marcus GM, et al. JAMA Cardiol. 2021 Nov 14. Doi: 10.1001/jamacardio.2021.5010.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Head-to-head: Efficacy of dabigatran versus warfarin on cognitive impairment Next Article
Network meta-analysis observes no clear effect of eicosapentaenoic acid on CV outcomes »
« Head-to-head: Efficacy of dabigatran versus warfarin on cognitive impairment Next Article
Network meta-analysis observes no clear effect of eicosapentaenoic acid on CV outcomes »
Table of Contents: AHA 2021
Featured articles
The scope of remote healthcare in hypertension and hyperlipidaemia
Atrial Fibrillation
New developments in remote diagnostics and monitoring of AF
Head-to-head: Efficacy of dabigatran versus warfarin on cognitive impairment
Posterior left pericardiotomy safe and effective in reducing atrial fibrillation
LAA ligation did not reduce recurrent atrial arrhythmias in persistent AF
Equal benefits of early rhythm control in AF subtypes
CVD Risk Reduction
Remote healthcare programme improves hypertension and lipid control
Novel oral PCSK9 inhibitor shows promising results for hypercholesterolaemia
REVERSE-IT: Interim analysis shows promising effect of bentracimab on ticagrelor reversal
No significant effect of aspirin on reducing cognitive impairment
Milvexian phase 2 data supports safety and efficacy for VTE prevention after total knee replacement
Network meta-analysis observes no clear effect of eicosapentaenoic acid on CV outcomes
Heart Failure
Empagliflozin efficacious in HF patients with preserved ejection fractions ≥50%
EMPULSE: Empagliflozin improves outcomes of acute heart failure
CHIEF-HF: Canagliflozin improves health status in heart failure
DREAM-HF: MPC therapy for HFrEF did not meet primary endpoint
Therapeutic approaches in heart failure with diabetes
Acute Coronary Syndrome
Ticagrelor cessation: early CABG non-inferior to delayed surgery
Distinguishing patients before AMI based on plaque morphology
Vascular Diseases: PVD
Rivaroxaban regimen beneficial after revascularisation for claudication
LIBERTY 360 shows quality-of-life improvements after peripheral vascular intervention
Deficient treatment outcomes after PVI in Black and low-income adults with PAD
REDUCE-IT: Cardiovascular risk reduction with icosapent ethyl in PAD
Vascular Diseases: CAD
Long-term reduced risk of CV events with ticagrelor plus aspirin after CABG
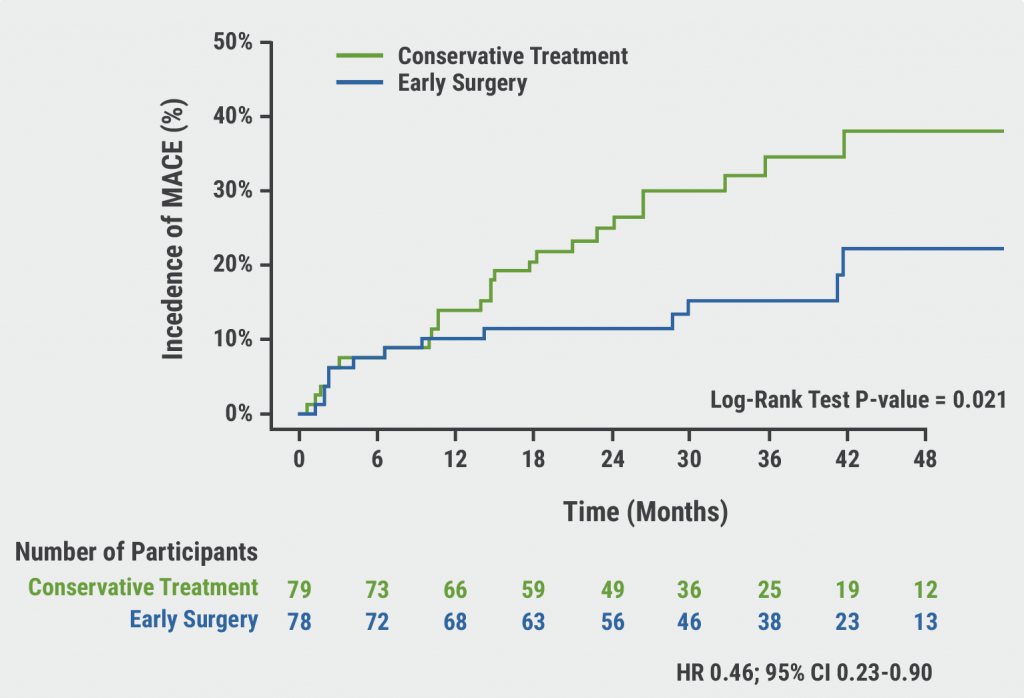
Early surgery outperforms conservative management in asymptomatic severe aortic stenosis
External support device for SVG grafts in CABG surgery shows promise
COVID-19 & the Heart
Blood pressure control disrupted during the pandemic
Icosapent ethyl did not reduce the risk of hospitalisation in COVID-19
Neutral effect of P2Y12 inhibitors in non-critical COVID-19 hospitalisations
COVID-19 mRNA vaccination benefits outweigh the risk for myocarditis
Other
2021 Guideline for Chest Pain: Top 10 takeaways
Accurate ejection fraction assessment in paediatric patients via artificial intelligence
Concomitant tricuspid annuloplasty reduces treatment failure in moderate tricuspid regurgitation
Related Articles
January 18, 2022
Letter from the Editor
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

