Dr Yujiro Yokoyama (St. Luke’s University Health Network, PA, USA) explained that most randomised clinical trials evaluating the effect of omega-3 fatty acid supplementation on cardiovascular risk reduction have shown neutral results [1]. Although a recent trial did show benefits of an EPA supplement in the secondary prevention of cardiovascular events, the suitability of the used placebo oil is a topic of discussion [2,3]. A network meta-analysis was conducted to examine the effect of EPA, docosahexaenoic acid (DHA), or EPA plus DHA on cardiovascular death, myocardial infarction, stroke, coronary revascularisation, and all-cause death. In total, 17 randomised controlled trials investigating 141,009 participants were included in the analysis.
In reducing cardiovascular death, the findings showed that EPA was more effective than mineral oil in (HR 0.80) in 1 analysis: a regimen of EPA plus DHA showed superiority in the prevention of cardiovascular death compared with olive oil (HR 0.93) and controls (HR 0.83). EPA versus placebo demonstrated neutral results in 6 other comparisons.
In reducing myocardial infarction, EPA was overall more effective than mineral oil regarding the reduction (HR 0.73). Eight comparisons demonstrated neutral results. Similarly, the occurrence of stroke was reduced in patients receiving EPA compared with patients receiving mineral oil (HR 0.74). Only 1 analysis found a reducing effect of EPA on stroke occurrence, whereas 8 other comparisons between EPA and placebo oils displayed neutral findings.
In reducing coronary revascularisation, EPA was more effective than EPA plus DHA (HR 0.67), corn oil (HR 0.63), mineral oil (HR 0.65), and olive oil (HR 0.66). Five analyses showed neutral results. Finally, no significant effect was found of EPA or EPA plus DHA on all-cause death versus placebo.
Although EPA outperformed a mineral oil placebo in the reduction of cardiovascular death, myocardial infarction, and stroke, the use of mineral oil as a placebo oil is questionable as mineral oil has been associated with increased apolipoprotein B, LDL cholesterol, and hs-CRP levels, and coronary artery plaque progression [2,4].
The observed effects of EPA on cardiovascular events are mostly neutral. Small beneficial effects of EPA have been observed for certain cardiovascular outcomes. However, the authors were unable to analyse participants with a low cardiovascular risk. Also, different regimens and doses of omega-3 fatty acids and placebo oils and heterogeneity in follow-up periods were reported. Therefore, a definite conclusion regarding the impact of EPA on cardiovascular outcomes cannot be made.
- Yokoyama Y, et al. Network Meta-Analysis of Randomized Controlled Trials of Eicosapentaenoic Acid for Cardiovascular Events Reduction. LF.RFO.13, AHA 2021 Scientific Sessions, 13–15 November.
- Bhatt DL, et al. N Engl J Med 2019;380(1):11–22.
- Sharma G, et al. JAMA. 2020;324(22):2262–2264.
- Budoff MJ, et al. Eur Heart J. 2020;41(40)3925–2932.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« New developments in remote diagnostics and monitoring of AF Next Article
Milvexian phase 2 data supports safety and efficacy for VTE prevention after total knee replacement »
« New developments in remote diagnostics and monitoring of AF Next Article
Milvexian phase 2 data supports safety and efficacy for VTE prevention after total knee replacement »
Table of Contents: AHA 2021
Featured articles
The scope of remote healthcare in hypertension and hyperlipidaemia
Atrial Fibrillation
New developments in remote diagnostics and monitoring of AF
Head-to-head: Efficacy of dabigatran versus warfarin on cognitive impairment
Posterior left pericardiotomy safe and effective in reducing atrial fibrillation
LAA ligation did not reduce recurrent atrial arrhythmias in persistent AF
Equal benefits of early rhythm control in AF subtypes
CVD Risk Reduction
Remote healthcare programme improves hypertension and lipid control
Novel oral PCSK9 inhibitor shows promising results for hypercholesterolaemia
REVERSE-IT: Interim analysis shows promising effect of bentracimab on ticagrelor reversal
No significant effect of aspirin on reducing cognitive impairment
Milvexian phase 2 data supports safety and efficacy for VTE prevention after total knee replacement
Network meta-analysis observes no clear effect of eicosapentaenoic acid on CV outcomes
Heart Failure
Empagliflozin efficacious in HF patients with preserved ejection fractions ≥50%
EMPULSE: Empagliflozin improves outcomes of acute heart failure
CHIEF-HF: Canagliflozin improves health status in heart failure
DREAM-HF: MPC therapy for HFrEF did not meet primary endpoint
Therapeutic approaches in heart failure with diabetes
Acute Coronary Syndrome
Ticagrelor cessation: early CABG non-inferior to delayed surgery
Distinguishing patients before AMI based on plaque morphology
Vascular Diseases: PVD
Rivaroxaban regimen beneficial after revascularisation for claudication
LIBERTY 360 shows quality-of-life improvements after peripheral vascular intervention
Deficient treatment outcomes after PVI in Black and low-income adults with PAD
REDUCE-IT: Cardiovascular risk reduction with icosapent ethyl in PAD
Vascular Diseases: CAD
Long-term reduced risk of CV events with ticagrelor plus aspirin after CABG
Early surgery outperforms conservative management in asymptomatic severe aortic stenosis
External support device for SVG grafts in CABG surgery shows promise
COVID-19 & the Heart
Blood pressure control disrupted during the pandemic
Icosapent ethyl did not reduce the risk of hospitalisation in COVID-19
Neutral effect of P2Y12 inhibitors in non-critical COVID-19 hospitalisations
COVID-19 mRNA vaccination benefits outweigh the risk for myocarditis
Other
2021 Guideline for Chest Pain: Top 10 takeaways
Accurate ejection fraction assessment in paediatric patients via artificial intelligence
Concomitant tricuspid annuloplasty reduces treatment failure in moderate tricuspid regurgitation
Related Articles
January 14, 2022
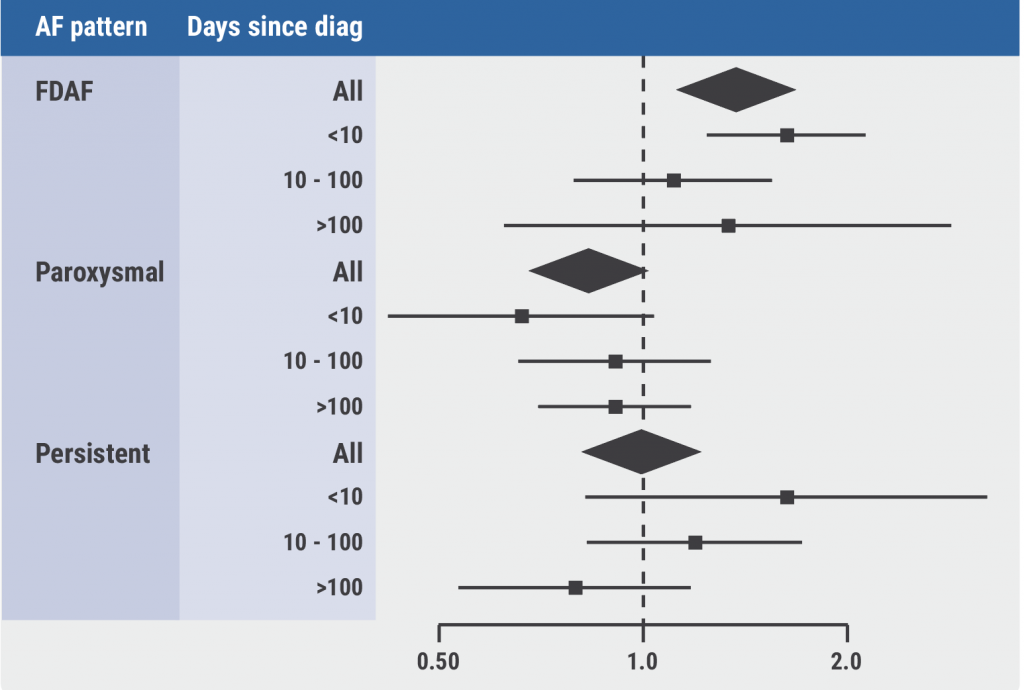
Equal benefits of early rhythm control in AF subtypes
January 14, 2022
Blood pressure control disrupted during the pandemic
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

