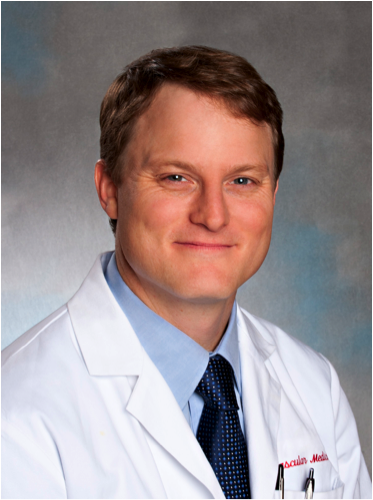
A remote, algorithm-driven programme with over 10,000 enrolled participants was able to reduce hypertension and LDL cholesterol in patients with a high risk for cardiovascular events. The programme may reduce the need for in-person visitations. Moreover, the remote programme could provide equitable care across underserved populations. Physician’s Weekly spoke with Dr Alexander Blood (Brigham and Women’s Hospital, MA, USA), the first author of the current study. The results of the remote healthcare programme were presented as a late-breaking abstract during the 2021 virtual meeting of the American Heart Association Scientific Sessions, 13–15 November [1].
 Dr Blood and colleagues developed a remote programme to improve hypertension and lipid control, with an emphasis on equal healthcare distribution across subgroups. Patient navigators, pharmacists, and digital technology were integrated into the programme’s model using a remote care delivery platform. In total, 6,887 patients were included in the lipid programme and 3,367 patients entered the hypertension programme. Approximately 40% of participants in either group completed the programme.
Dr Blood and colleagues developed a remote programme to improve hypertension and lipid control, with an emphasis on equal healthcare distribution across subgroups. Patient navigators, pharmacists, and digital technology were integrated into the programme’s model using a remote care delivery platform. In total, 6,887 patients were included in the lipid programme and 3,367 patients entered the hypertension programme. Approximately 40% of participants in either group completed the programme.Systolic blood pressure (BP), in mmHg, was reduced at the last measurement of the study (mean 135) compared with baseline (mean 145; P<0.0001) in all patients who were enrolled in the hypertension programme. This effect was more pronounced in patients who completed the programme (mean 125 vs mean 137; P<0.0001). Similarly, diastolic BP was significantly decreased at the latest BP measurement of the study compared with baseline. In addition, 92% of the patients who completed the programme reached their guideline-recommended BP goals. Subgroup analysis demonstrated that the effect was consistent across ethnic groups, with equal proportions of subgroup populations achieving study completion. This result suggests that traditionally underserved subgroups benefit equally from the current programme.
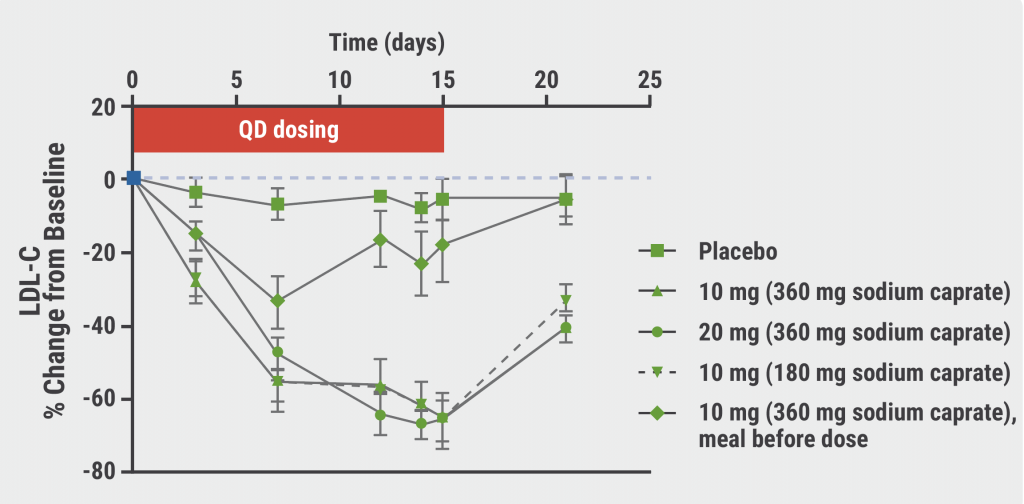
The lipid programme showed a reduction of LDL cholesterol, in mg/dL, at the latest performed measurement (mean 100) compared with baseline (mean 145; P<0.0001). Again, this effect was more pronounced in patients who completed the programme (mean 70 vs mean 140; P<0.0001). Reductions in LDL cholesterol were also similar across subgroups.
Physician’s Weekly interviewed Dr Blood to discuss the possibilities of this novel algorithm-driven healthcare programme.
Physician’s Weekly: Could you explain the remote healthcare programme that was developed for the current study?
We were aiming to provide an end-to-end service model to move the needle for a large population of patients with hypertension or hyperlipidaemia. The model managed patients with these chronic diseases remotely, on a large scale. We consider our study to be a clinical implementation study, analogous to a warfarin clinic or dialysis clinic, in which information is communicated back to primary care.
Patients received a connected blood pressure cuff, via which data was sent to their electronic health record. Subsequently, patients received the best recommendation based on lab values, demographics, and medical history. If needed, therapy could be initiated, intensified, and monitored. For safety reasons, lab values were continuously monitored. Besides this, the process was fairly flexible.
We could initiate a new line of therapy for a couple of weeks and monitor adverse events and blood pressure. The data was integrated, and the effectiveness of the therapy was analysed. Subsequent decisions were made based on these results. In addition, regular follow-up was important to make sure that patients were adherent to therapy and optimised the use of combination pills. By prescribing generic medicine and using our patients' preferred pharmacies we reduced the costs and effort for our patients. In addition, diet and lifestyle recommendations were part of the package. We provided advice for every patient that entered the programme. The overall goal was to help patients reduce their overall cardiovascular risk and help them to achieve their guideline-directed targets.
Physician’s Weekly: What are the main advantages and disadvantages of this approach?
Importantly, our approach was not onerous on the patients or the providers. One of the major challenges for patients is getting to a healthcare facility. It takes time, effort, and money. With the current approach, we met patients where they were. If a patient had given permission to use emails or text messages, the appropriate healthcare could be delivered almost completely asynchronously. Patients measured their blood pressure when they were able, at home, or at the workplace. That data automatically gets integrated and sent over to us.
Next, approximately 80–90% of the people who completed our programme reached their guideline-recommended targets. In addition, when we monitor these patients in maintenance, they may remain at their targets in the long term. I think our study has shown that we can unburden the system and manage a large volume of patients with our approach. Moreover, since most individuals around the world have access to a mobile phone and telephone calls have been our default communication option, this approach could be scaled up to a much greater capacity. Notably, I think that our approach can deliver guideline-directed care to patients with limited access to healthcare facilities, thereby reducing barriers and disparities in care.
On the downside, our system is not the perfect solution for a hundred percent of the patients. Not all patients are comfortable using text messages, secure patient gateway email, or telephones. In 5–10% of the cases, we need to rely on traditional outpatient visitations.
Physician’s Weekly: What was the role of the so-called navigators that were part of the programme?
The navigators were unlicensed, mostly college-educated individuals with an interest in medicine. They received a tailored training from pharmacists and clinicians to answer the most frequently asked questions by our patients. There was always a pharmacist or clinician available to answer the complicated or unfrequently asked questions, but the navigators were the first line of contact.
Physician’s Weekly: Were there other control mechanisms installed in the programme?
Next to the navigator-pharmacist-clinician axis, the software we used is designed to detect irregular patterns in a patient’s profile. The pharmacist or clinician can respond to these signs if needed. Furthermore, weekly meetings were organised to review all patients who were in the system and getting therapy. All the prescriptions, lab values, and adverse events were addressed and controlled. Finally, a daily report was conducted on the approximately 420,000 blood pressure measurements that came in. A nurse practitioner monitored this report and controlled for divergent blood pressures. Subsequently, outlying values could be addressed by the clinician.
- Blood AJ, et al. Digital Care Transformation: Report from the First 10,000 Patients Enrolled in a Remote Algorithm-based Cardiovascular Risk Management Program to Improve Lipid and Hypertension Control. LBS02, AHA Scientific Sessions 2021, 13–15 November.
Posted on
Previous Article
« Telehealth exercise and diet programs curb pain and boost function in knee osteoarthritis Next Article
Atezolizumab, nivolumab tied to longer survival than docetaxel in advanced lung cancer »
« Telehealth exercise and diet programs curb pain and boost function in knee osteoarthritis Next Article
Atezolizumab, nivolumab tied to longer survival than docetaxel in advanced lung cancer »
Table of Contents: AHA 2021
Featured articles
The scope of remote healthcare in hypertension and hyperlipidaemia
Atrial Fibrillation
New developments in remote diagnostics and monitoring of AF
Head-to-head: Efficacy of dabigatran versus warfarin on cognitive impairment
Posterior left pericardiotomy safe and effective in reducing atrial fibrillation
LAA ligation did not reduce recurrent atrial arrhythmias in persistent AF
Equal benefits of early rhythm control in AF subtypes
CVD Risk Reduction
Remote healthcare programme improves hypertension and lipid control
Novel oral PCSK9 inhibitor shows promising results for hypercholesterolaemia
REVERSE-IT: Interim analysis shows promising effect of bentracimab on ticagrelor reversal
No significant effect of aspirin on reducing cognitive impairment
Milvexian phase 2 data supports safety and efficacy for VTE prevention after total knee replacement
Network meta-analysis observes no clear effect of eicosapentaenoic acid on CV outcomes
Heart Failure
Empagliflozin efficacious in HF patients with preserved ejection fractions ≥50%
EMPULSE: Empagliflozin improves outcomes of acute heart failure
CHIEF-HF: Canagliflozin improves health status in heart failure
DREAM-HF: MPC therapy for HFrEF did not meet primary endpoint
Therapeutic approaches in heart failure with diabetes
Acute Coronary Syndrome
Ticagrelor cessation: early CABG non-inferior to delayed surgery
Distinguishing patients before AMI based on plaque morphology
Vascular Diseases: PVD
Rivaroxaban regimen beneficial after revascularisation for claudication
LIBERTY 360 shows quality-of-life improvements after peripheral vascular intervention
Deficient treatment outcomes after PVI in Black and low-income adults with PAD
REDUCE-IT: Cardiovascular risk reduction with icosapent ethyl in PAD
Vascular Diseases: CAD
Long-term reduced risk of CV events with ticagrelor plus aspirin after CABG
Early surgery outperforms conservative management in asymptomatic severe aortic stenosis
External support device for SVG grafts in CABG surgery shows promise
COVID-19 & the Heart
Blood pressure control disrupted during the pandemic
Icosapent ethyl did not reduce the risk of hospitalisation in COVID-19
Neutral effect of P2Y12 inhibitors in non-critical COVID-19 hospitalisations
COVID-19 mRNA vaccination benefits outweigh the risk for myocarditis
Other
2021 Guideline for Chest Pain: Top 10 takeaways
Accurate ejection fraction assessment in paediatric patients via artificial intelligence
Concomitant tricuspid annuloplasty reduces treatment failure in moderate tricuspid regurgitation
Related Articles
January 14, 2022
New developments in remote diagnostics and monitoring of AF
January 18, 2022
Letter from the Editor
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

