https://doi.org/10.55788/aa8402fa
“Quick and adequate decongestion in patients with acute HF remains difficult in today’s practice,” said Dr Jozine ter Maaten (University of Groningen, the Netherlands) [1]. “The one-size-fits-all approach that is used falls short in many patients.” Urinary sodium (natriuresis) may guide diuretic therapy to personalise therapy and improve decongestion. The pragmatic, single-centre, open-label, randomised-controlled PUSH-AHF trial (NCT04606927) assessed the effectiveness and safety of natriuresis-guided diuretic therapy in acute HF. Participants in the experimental arm (n=150) received a standardised starting dose of loop diuretics based on renal function and outpatient dose. If the dose was insufficient, defined as urinary sodium <70 mmol/L and diuresis <150 mL/hour, the bolus dose was doubled. If this still proved to be insufficient, hydrochlorothiazide, acetazolamide, or an SGLT2 inhibitor was added. Participants in the control arm (n=160) received the standard-of-care. The dual primary endpoints were 24-hour natriuresis and 180-day all-cause mortality or adjudicated HF hospitalisation.
The first primary endpoint was met, in favour of the natriuresis-guided arm, with an estimated difference of 63 mmol/L urinary sodium at 24 hours (95% CI 18–109; P=0.0061). The second primary endpoint was not met (HR 0.92; 95% CI 0.62–1.38; P=0.70). The effect of natriuresis-guided therapy on natriuresis was maintained at 48 hours (P=0.024). Furthermore, diuresis was improved at both 24 hours (P=0.0053) and 48 hours (P=0.014) in the experimental arm. Dr ter Maaten emphasised that natriuresis-guided therapy did not lead to electrolyte disorders or higher rates of renal or cardiac adverse events.
In summary, natriuresis-guided diuretic therapy was safe, improved natriuresis and diuresis in patients with acute HF. There was, however, no effect of this intervention on 180-day all-cause mortality or adjudicated HF hospitalisation. “The results of this trial are directly applicable as spot urinary sodium values are inexpensive and easy to obtain, as are the medications used in the treatment algorithm,” argued Dr ter Maaten. “Finally, these findings underscore the use of repeated spot urinary sodium assessments for personalised treatment targets as proposed by the ESC HF guidelines.”
- Ter Maaten JM, et al. The pragmatic urinary sodium-based treatment algorithm in acute heart failure (PUSH-AHF) trial. Hot Line Session 8, ESC Congress 2023, 25–28 August, Amsterdam, the Netherlands.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« Guidelines for Acute Coronary Syndrome Next Article
Results of FRAIL-AF trial suggest increased bleeding risk with DOACs »
« Guidelines for Acute Coronary Syndrome Next Article
Results of FRAIL-AF trial suggest increased bleeding risk with DOACs »
Table of Contents: ESC 2023
Featured articles
How to manage arterial thrombosis and thromboembolism in COVID-19?
2023 ESC Guidelines & Updates
Heart failure: the 2023 update
Guidelines for Acute Coronary Syndrome
Guidelines for the management of cardiomyopathies
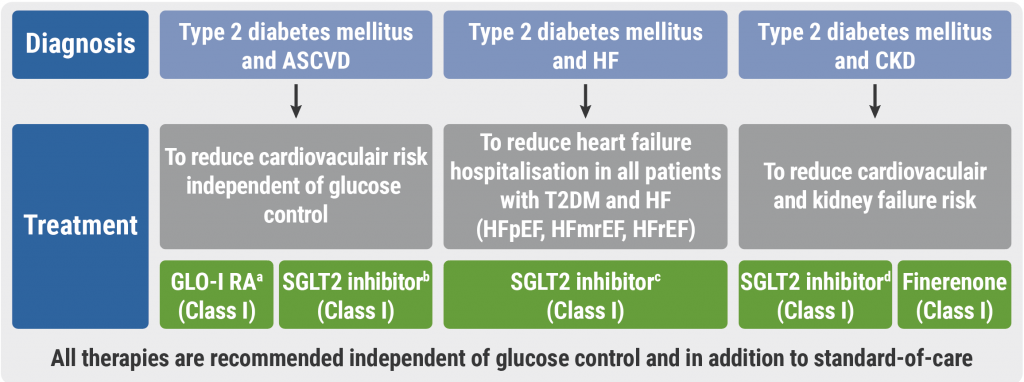
Cardiovascular disease and diabetes: new guidelines
Guidelines for the management of endocarditis
Trial Updates in Heart Failure
Traditional Chinese medicine successful in HFrEF
CRT upgrade benefits patients with HFrEF and an ICD
Catheter ablation saves lives in end-stage HF with AF
Meta-analysis: Does FCM improve clinical outcomes in HF?
HEART-FID: Is intravenous ferric carboxymaltose helpful in HFrEF with iron deficiency?
Natriuresis-guided diuretic therapy to facilitate decongestion in acute HF
DICTATE-AHF: Early dapagliflozin to manage acute HF
STEP-HFpEF: Semaglutide safe and efficacious in HFpEF plus obesity
Key Research on Prevention
Does colchicine prevent perioperative AF and MINS?
Diagnostic tool doubles cardiovascular diagnoses in patients with COPD or diabetes
Inorganic nitrate strongly reduces CIN in high-risk patients undergoing angiography
Finetuning Antiplatelet and Anticoagulation Therapy
Should we use anticoagulation in AHRE to prevent stroke?
Results of FRAIL-AF trial suggest increased bleeding risk with DOACs
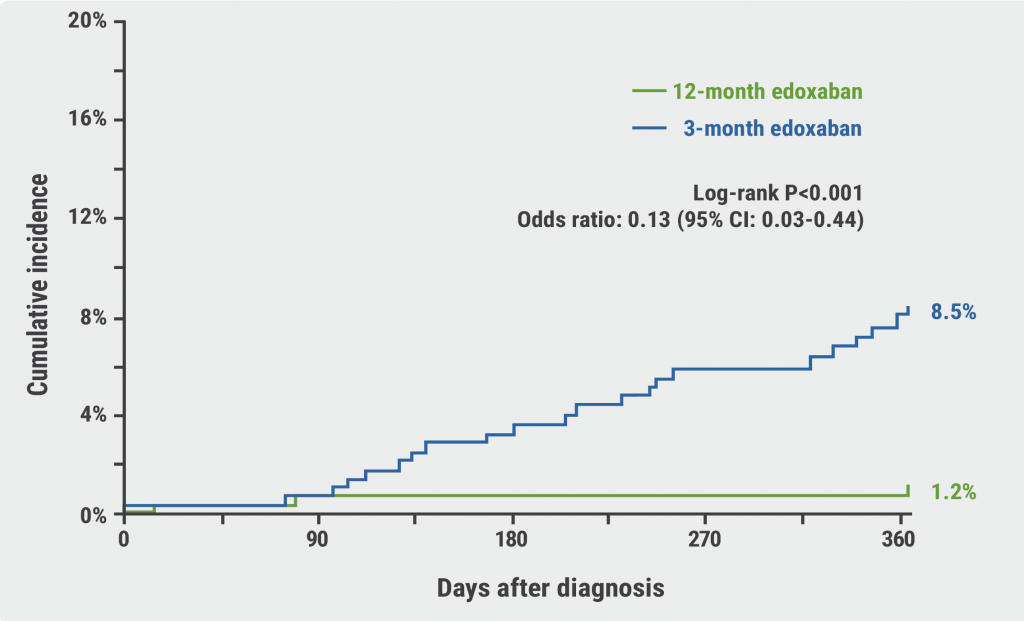
The optimal duration of anticoagulation therapy in cancer patients with DVT
DAPT or clopidogrel monotherapy after stenting in high-risk East-Asian patients?
Assets for ACS and PCI Optimisation
Immediate or staged revascularisation in STEMI plus multivessel disease?
Lp(a) and cardiovascular events: which test is the best?
No benefit of extracorporeal life support in MI plus cardiogenic shock
Functional revascularisation outperforms culprit-only strategy in older MI patients
Can aspirin be omitted after PCI in patients with high bleeding risk?
Angiography vs OCT vs IVUS guidance for PCI: a network meta-analysis
OCTOBER trial: OCT-guided PCI improves clinical outcomes in bifurcation lesions
Other
Minimising atrial pacing does not reduce the risk for AF in sinus node disease
ARAMIS: Can anakinra alleviate acute myocarditis?
Expedited transfer to a specialised centre does not improve cardiac arrest outcomes
Acoramidis improves survival and functional status in ATTR-CM
Related Articles
October 30, 2023
Cardiovascular disease and diabetes: new guidelines
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

