Medicom: Could you explain the need for new guidelines on antithrombotic therapy in patients with COVID-19?

“The association between venous thromboembolism and COVID-19 has been well recognised, and numerous guidelines have addressed this matter,” outlined Dr Lip.
“However, there is still an unmet need in patients who develop arterial thrombosis or thromboembolism during the course of COVID-19. We need to establish how to deal with patients who develop an acute coronary syndrome in the course of acute illness, including the use of PCI and stenting. Also, there are patients who develop an acute ischemic stroke; how do we manage these patients? Furthermore, we need to address patients with a particular risk for arterial thromboembolism during COVID-19, such as those with atrial fibrillation or peripheral artery disease, and agree on which steps to take in the context of associated antithrombotic therapies.”
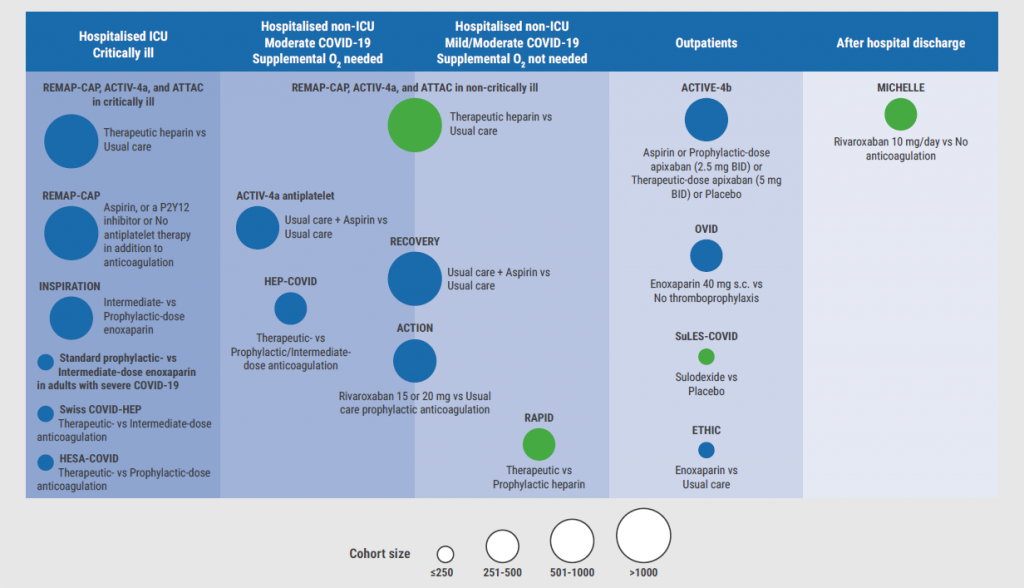
“Finally, different recommendations are needed for the outpatient setting, the non-ICU and ICU setting, and so forth (see Figure). Therefore, CHEST convened the expert panel and produced this guideline. I’m very pleased to see the final report, of which I had the honour and pleasure to be the senior author.”
Medicom: Were you able to fill some of the existing gaps in the literature or identify where the level of evidence is adequate to be applied?
“The good thing about CHEST expert panel reports and guidelines is that we conduct a systematic review of the existing literature,” Dr Lip replied. “There were no large, randomised trials in the specific populations we aimed to analyse. Therefore, we mostly depended on cohort studies and extrapolation of evidence from non-COVID populations. In addition, we drew on the experience of the multidisciplinary panel. Hopefully, the report will be a useful resource for healthcare practitioners who deal with patients who are at risk of, or develop, arterial thrombosis or thromboembolism during COVID-19. It is good to be well prepared before the winter comes.”
Figure: Antithrombotic therapy in arterial thrombosis and thromboembolism in COVID-19. Kindly provided by Dr Lip.
Medicom: There are prevention and prophylaxis elements in the report. Could you discuss some of the key recommendations?
“I’ll take atrial fibrillation as an example, because it’s a common condition and it has been associated with many comorbidities,” argued Dr Lip. “These patients are at risk of experiencing complications during COVID-19.”
“If they’re managed and in a non-hospitalised setting, and if they already take an oral anticoagulant for atrial fibrillation, the recommendation is to continue with the oral anticoagulation. If they’re hospitalised with COVID-19 and develop new onset atrial fibrillation in the non-ICU setting, perhaps an oral anticoagulant would suffice. Therapeutic anticoagulation with either a DOAC or a vitamin K antagonist could be used for this matter. In the ICU setting, patients may not be able to take oral anticoagulation. Therefore, parenteral anticoagulation may be required. When patients with atrial fibrillation are discharged, one must look at the various factors related to the use of anticoagulants in this population. If these patients have a CHA2DS2-VASc score of 2 or higher they clearly need long-term oral anticoagulation, and perhaps visit a specialist on how to manage them subsequently. This is one example where prophylaxis for atrial fibrillation is being administered before the patient is admitted to the hospital. On the other hand, there is the scenario of being admitted to the hospital with an acute illness and developing de novo atrial fibrillation.”
“Another scenario we have covered is the situation where a patient is admitted to the hospital with COVID-19 and then sustains an acute stroke,” Dr Lip continued. “This urgent matter needs to be managed appropriately. In the case of recanalisation therapy, whether it’s thrombolysis or thrombectomy, this requires consultation with a vascular neurologist. If a patient who has had a previous stroke and received antiplatelet therapy for this is admitted to the hospital with COVID-19, the general recommendation is to continue antiplatelet therapy. Depending on the particular setting, prophylactic low-molecular-weight heparin is required during the patient’s time in hospital.”
Medicom: What about patients with peripheral artery disease? This must be a unique subset of patients as well?
“There are patients with chronic peripheral artery disease that are taking antiplatelet therapies. If they are admitted to the hospital with COVID-19, an additional prophylactic dose of low-molecular-weight heparin may be recommended next to the antiplatelet therapy, given the potential risk of thrombosis with COVID-19. Some patients with peripheral artery disease will develop acute life-threatening ischaemia during their hospital stay. This situation requires the efforts of a multidisciplinary team and a vascular specialist, who need to decide whether or not there is a need for acute revascularisation.”
“In summary, on the one hand, there is the difficulty of not having large, randomised trials for the specific populations we investigated. On the other hand, by extrapolating the best evidence from non-COVID-19 scenarios and adapting it to COVID-19 admissions, hopefully, we have delivered some useful recommendations.”
Medicom: Many studies are ongoing in this area. Can you discuss some of the results you’re looking forward to?
“There are some areas for which we would like to see more evidence,” said Dr Lip. “I’ll give one example. Recently, data from the C19-ACS trial have been published [2]. This trial investigated the combination of a low-dose DOAC plus aspirin in a COVID-19 population. We know from the non-COVID-19 trials named COMPASS and ATLAS that, in patients at risk of arterial thromboembolism, low-dose rivaroxaban plus aspirin offers benefits for patients. We conducted the C19-ACS trial to try and test that regimen in patients with COVID-19 [3,4]. Unfortunately, we had to stop the trial because we couldn’t recruit enough patients. Nonetheless, I think this question needs to be resolved.”
Medicom: Do you have any final comments or recommendations for your fellow physicians?
“We are now getting used to living with COVID-19 in the background, the same way as we’ve been living with influenza for many years. COVID-19 is not going to disappear. In the early days, the situation was bad because of the high risk of thromboembolism that is associated with COVID-19 towards the more severe end of the spectrum.
For patients at risk of developing arterial thromboembolism, we now have a resource that provides guidance on how to manage these patients,” Dr Lip concluded.
- Potpora T, et al. Chest. 2023;S0012-3692(23)00938-8.
- Kanagaratnam P, et al. J Thromb Haemost. 2023 Aug;21(8):2213-2222.
- Eikelboom JW, et al. N Engl J Med. 2017;377:1319-1330.
- Mega JL, et al. N Engl J Med. 2012;366:9-19.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« What every doctor should know about CLL in today’s treatment landscape Next Article
Gentamicin improves symptoms in paediatric Nagashima-type palmoplantar keratosis »
« What every doctor should know about CLL in today’s treatment landscape Next Article
Gentamicin improves symptoms in paediatric Nagashima-type palmoplantar keratosis »
Table of Contents: ESC 2023
Featured articles
How to manage arterial thrombosis and thromboembolism in COVID-19?
2023 ESC Guidelines & Updates
Heart failure: the 2023 update
Guidelines for Acute Coronary Syndrome
Guidelines for the management of cardiomyopathies
Cardiovascular disease and diabetes: new guidelines
Guidelines for the management of endocarditis
Trial Updates in Heart Failure
Traditional Chinese medicine successful in HFrEF
CRT upgrade benefits patients with HFrEF and an ICD
Catheter ablation saves lives in end-stage HF with AF
Meta-analysis: Does FCM improve clinical outcomes in HF?
HEART-FID: Is intravenous ferric carboxymaltose helpful in HFrEF with iron deficiency?
Natriuresis-guided diuretic therapy to facilitate decongestion in acute HF
DICTATE-AHF: Early dapagliflozin to manage acute HF
STEP-HFpEF: Semaglutide safe and efficacious in HFpEF plus obesity
Key Research on Prevention
Does colchicine prevent perioperative AF and MINS?
Diagnostic tool doubles cardiovascular diagnoses in patients with COPD or diabetes
Inorganic nitrate strongly reduces CIN in high-risk patients undergoing angiography
Finetuning Antiplatelet and Anticoagulation Therapy
Should we use anticoagulation in AHRE to prevent stroke?
Results of FRAIL-AF trial suggest increased bleeding risk with DOACs
The optimal duration of anticoagulation therapy in cancer patients with DVT
DAPT or clopidogrel monotherapy after stenting in high-risk East-Asian patients?
Assets for ACS and PCI Optimisation
Immediate or staged revascularisation in STEMI plus multivessel disease?
Lp(a) and cardiovascular events: which test is the best?
No benefit of extracorporeal life support in MI plus cardiogenic shock
Functional revascularisation outperforms culprit-only strategy in older MI patients
Can aspirin be omitted after PCI in patients with high bleeding risk?
Angiography vs OCT vs IVUS guidance for PCI: a network meta-analysis
OCTOBER trial: OCT-guided PCI improves clinical outcomes in bifurcation lesions
Other
Minimising atrial pacing does not reduce the risk for AF in sinus node disease
ARAMIS: Can anakinra alleviate acute myocarditis?
Expedited transfer to a specialised centre does not improve cardiac arrest outcomes
Acoramidis improves survival and functional status in ATTR-CM
Related Articles
October 30, 2023
ARAMIS: Can anakinra alleviate acute myocarditis?
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

