A large and unmet need exists for a more effective therapy in the management of HS. An interesting novel agent under investigation is the nanobody sonelokimab, a humanised antibody targeting IL-17A and IL-17F. Increasing evidence highlights IL-17A and IL-17F-mediated inflammation in HS pathogenesis. “Some patients go on to develop tunnels and draining fistulas. And we know that IL-17A and IL-17F are even higher in those with tunnels compared with patients that don’t develop tunnels,” Prof. Brian Kirby (St. Vincent´s University Hospital, Ireland) explained [1]. In addition, there is an albumin-binding domain. Due to its small molecular size and its ability to bind to albumin, sonelokimab is able to penetrate inflamed tissue which is otherwise difficult-to-treat; thus, directly targeting the site of inflammation.
Prof. Kirby presented the 12-week results of the double-blind, placebo-controlled, phase 2 MIRA trial (NCT05322473). This trial included adult patients with HS, Hurley stage II/III, a total abscess and/or inflammatory nodule count of ≥5, and the presence of HS lesions in ≥2 anatomical regions. They received either 120 mg or 240 mg sonelokimab, placebo, or adalimumab as an active comparator (to validate clinical findings but not powered for any statistical comparison). The primary study endpoint was the proportion of participants achieving a ≥75% reduction in total nodule counts from baseline with no new abscess or tunnel draining count (i.e. HiSCR 75).
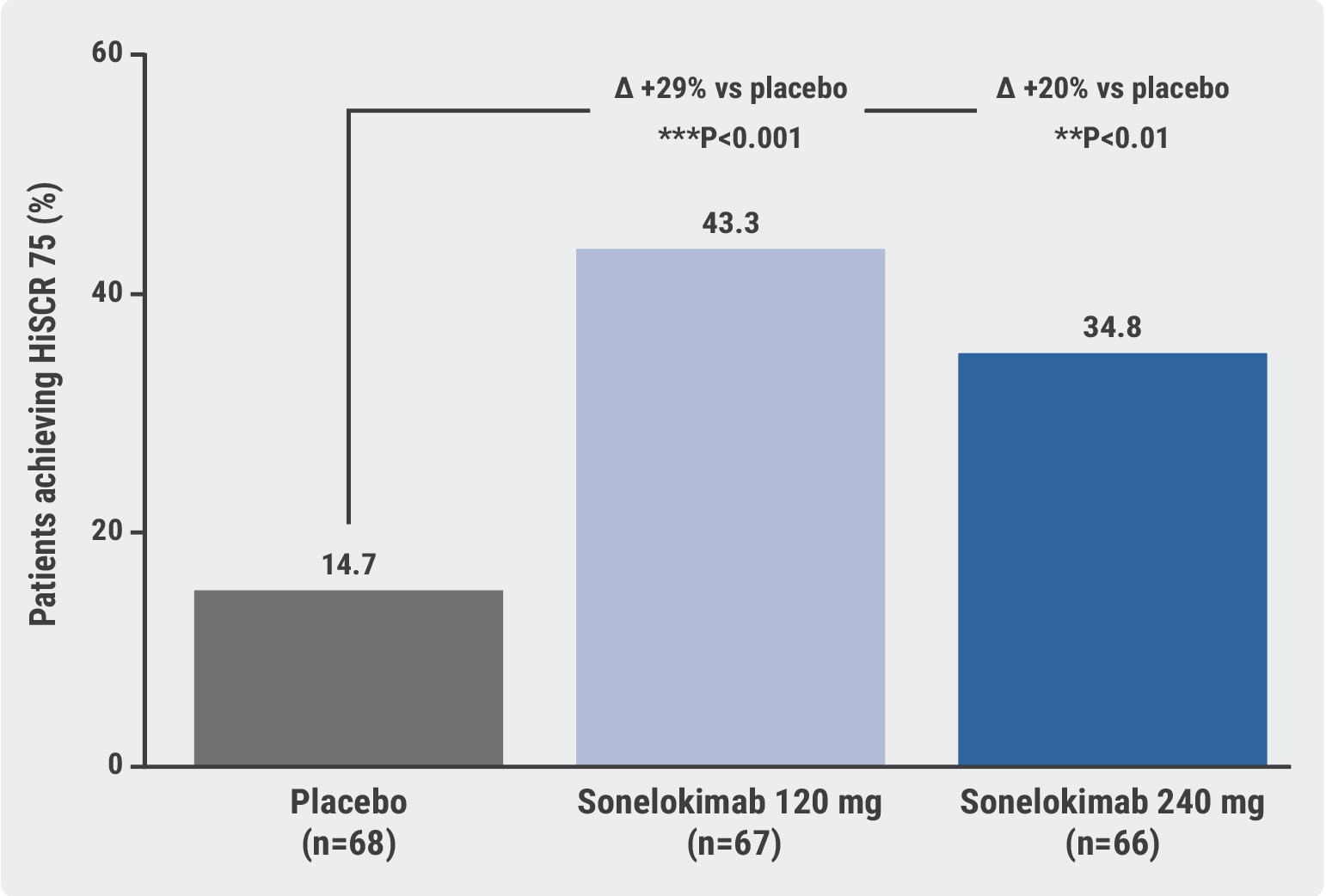
All in all, 234 participants could be included and >95% completed week 12. Significantly more participants treated with sonelokimab achieved the primary endpoint at week 12 compared with placebo (43.3% treated with 120 mg and 34.8% treated with 240 mg vs 14.7% in the placebo group; P<0.001 for the first and P<0.01 for the second comparison; see Figure).
Figure: Sonelokimab met the primary endpoint of HiSCR75 at week 12 [1]
“Sonelokimab works quickly. We see significant differences versus placebo as early as week 8,” Prof. Kirby said. Moreover, sonelokimab improved quality of life, as measured by the Dermatology Life Quality Index (DLQI; i.e. improvement of ≥4 points, which is considered clinically relevant) and led to less skin pain.
The nanobody was well tolerated in accordance with its known safety profile. Candida infections occurred more frequently in the sonelokimab groups (e.g. 6% cases of oral candidiasis in the low-dose group and 12.1% in the high-dose group compared with no cases in the placebo group) but were generally mild-to-moderate and did not lead to treatment withdrawal.
- Kirby B, et al. Efficacy and safety of the IL-17A- and IL-17F-inhibiting Nanobody® Sonelokimab in patients with active, moderate-to-severe hidradenitis suppurativa: Results from the global, randomized, double-blind, placebo-controlled phase 2 MIRA trial. D1T01.1H, EADV Congress 2023, 11–14 October, Berlin, Germany.
Copyright ©2023 Medicom Medical Publishers
Posted on

