Associations between HS and various autoimmune conditions including inflammatory bowel diseases or spondyloarthropathies have been reported in the past. A new population-based study focused on the possibility that HS may also be linked to autoimmune pathologies of connective tissue disease (CTD). Data was retrieved from claims files of non-governmental health insurance from 31 December 2002 to 31 December 2017 in the USA. Included were patients with a diagnosis of HS that were compared with a group of non-HS patients with similar risk profiles and comorbidity. The study population included 66,448 patients with and without HS with a mean age of 37 years. About 3 quarters of patients were female, and comorbidities in terms of IBD, psoriasis, or arthritis ranged between 0.7% and 1.2% with a similar distribution of diagnoses in both groups. The median follow-up time was 533 days in the HS group and 545 days in the non-HS group. Follow-up was terminated in case of a first event of new diagnosis of CTD, death, disenrollment, or end of data stream. Non-biologic immune-modulatory treatment was taken by 1.4% in both groups, and biologics were prescribed to 0.9% of patients in the HS group and 0.6% in the non-HS group.
Hazard ratios (HR) for developing systemic sclerosis (HR 0.9), systemic vasculitis (HR 0.87) or Sjögren’s syndrome (HR 0.9) were not elevated. However, a substantial association was found for HS and SLE (HR 1.63). The risk of being diagnosed with morphoea when suffering from HS was doubled (HR 2.02) compared with a patient with a comparable risk profile without HS. The investigators deemed it most likely that SLE was newly appearing instead of already co-existing, as a Kaplan-Meier analysis discovered a maintained relationship between HS and SLE.
- Schneeweiss MC, et al. P18695, AAD Virtual Meeting Experience, 12-14 June 2020.
- Schneeweiss MC, et al. J Eur Acad Dermatol Venereol. June 2020. Doi:10.1111/jdv.16728.
Posted on
Previous Article
« Biologics in HS – a growing armamentarium Next Article
Intranasal kappa-opioid agonist effective for intractable pruritus »
« Biologics in HS – a growing armamentarium Next Article
Intranasal kappa-opioid agonist effective for intractable pruritus »
Table of Contents: AAD 2020
Featured articles
Late-Breaking Abstracts
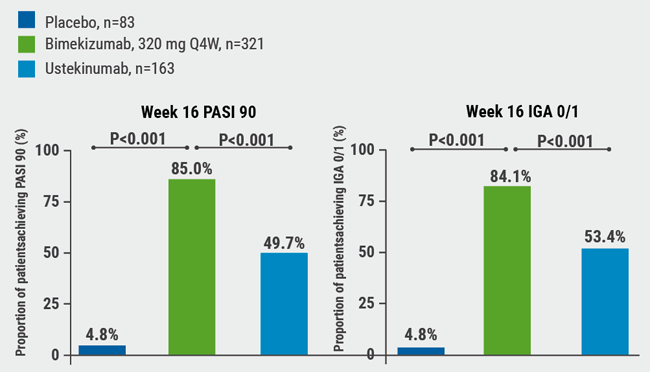
IL-17A and IL-17F blockade remarkably effective in psoriasis
Good response and pruritus reduction in AD with novel selective JAK1 inhibitor
Novel IL-23 blocker risankizumab highly effective and tolerable in psoriasis
Tape stripping – a painless way to distinguish AD and psoriasis?
IL-4/IL-13 blocker dupilumab effective in children with severe AD
Pembrolizumab leads to higher toxicity risk in obese melanoma patients
Can gene expression help to pick the right biologic to treat psoriasis in cancer patients?
Omalizumab for cancer-induced dermatoses
Psoriasis – What Is Hot?
Psoriasis therapy for children and pregnancies
Biologic psoriasis treatment to lower cardiovascular risk?
Systemic Therapies for Dermatologists
How to manage cutaneous side effects of immunotherapy
Cannabinoids: a future role in dermatology?
Hidradenitis Suppurativa/Acne Inversa
Biologics in HS – a growing armamentarium
Pearls of the Posters
Selective IL-23 blocker safe in elderly psoriasis patients
Spironolactone safe for androgenetic alopecia in cancer survivors
Baricitinib beneficial in head and neck AD
ECLIPSE trial: skin clearance independent of PsA status at baseline
Related Articles
August 19, 2020
Selective IL-23 blocker safe in elderly psoriasis patients
August 6, 2020
IL-17A and IL-17F blockade remarkably effective in psoriasis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

