"Our findings should provide reassurance to rheumatologists, other health professionals and vaccine recipients, and promote confidence in the safety of COVID-19 vaccination in people with inflammatory rheumatic diseases," Dr. Pedro Machado of University College London told Reuters Health by email.
"While the study was not aimed at identifying predictors of flare in patients with inflammatory rheumatic diseases, we observed a low flare rate, particularly severe flares (0.6%)," he noted. "The percentage of flares was slightly higher in patients with moderate/high disease activity (5.2%) compared with patients in remission/low disease activity, raising the possibility of an association between higher disease activity and higher flare rate."
"However, it is important to note that flares can occur as part of the natural history of the disease," he said, "and the observed percentages of flare would be compatible with the natural history of the disease rather than necessarily caused by vaccines against SARS-CoV-2."
As reported in Annals of the Rheumatic Diseases, Dr. Machado and colleagues analyzed data on 5,121 patients with rheumatic and musculoskeletal diseases (RMD) from 30 countries, 90% of whom (mean age, 60.5; 68%, women) had inflammatory/autoimmune RMD (I-RMDs). The authors note that patients with I-RMDs were excluded from the vaccine clinical development programs, and previous studies in these patients were small.
Participants (10%) with noninflammatory (NI)-RMDs had a mean age of 72.4 and 77% were women.
Overall, the most frequent conditions were inflammatory joint diseases (58%), connective tissue diseases (18%) and vasculitis (12%). Fifty-four percent of patients "54% received conventional synthetic disease-modifying antirheumatic drugs (DMARDs); 42% biological DMARDs; and 35% immunosuppressants (in combination with other medications).
Most patients received the Pfizer/BioNTech vaccine (70%), followed by AstraZeneca/Oxford (17%) and Moderna (8%).
Among those who were fully vaccinated, breakthrough infections were reported in 0.7% of I-RMD patients and 1.1% of NI-RMD patients.
I-RMD flares occurred in 4.4% of patients (0.6% severe), with 1.5% resulting in medication changes.
Adverse events (AEs) were reported in 37% of I-RMD and 40% of NI-RMD cases; serious AEs occurred in 0.4% I-RMD and 1.9% NI-RMD patients.
The authors conclude, "The safety profiles of SARS-CoV-2 vaccines in patients with I-RMD was reassuring and comparable with patients with NI-RMDs. The majority of patients tolerated their vaccination well with rare reports of I-RMD flare and very rare reports of serious AEs."
Dr. Machado said, "Our data will support discussions about the safety and positive benefit/risk ratio of COVID-19 vaccination for people with inflammatory rheumatic diseases. This information will also help support the development of new and updated recommendations by competent organizations."
Dr. Wen-Hai Shao, an associate professor in the Division of Immunology, Allergy and Rheumatology at the University of Cincinnati in Ohio commented on the study in an email to Reuters Health. "DMARDs are much milder than immunosuppressants, (so) the key is those patients on immunosuppressants; however, the article didn't provide separate information on this group."
"Patients on drugs that target the adaptive immune system and the innate immune system should be analyzed separately," he said. "In addition, a lot of information is (missing)." For example, he said, How do the data compare to healthy individuals? What was the disease status when vaccination was given? What were the type and doses of drugs given? Did patients have other diseases, as well?
"A bioinformatics approach could be used to analyze the data in these different ways," Dr. Shao concluded.
SOURCE: https://bit.ly/3GZJNnS Annals of the Rheumatic Diseases, online December 31, 2021.
By Marilynn Larkin
Posted on
Previous Article
« Risk of MS relapse high when natalizumab is stopped for pregnancy Next Article
AI can identify, grade prostate cancer like a pathologist »
« Risk of MS relapse high when natalizumab is stopped for pregnancy Next Article
AI can identify, grade prostate cancer like a pathologist »
Related Articles
September 4, 2019
What is new in osteoarthritis
January 25, 2022
Allopurinol treatment for gout appears safe in kidney patients
September 4, 2019
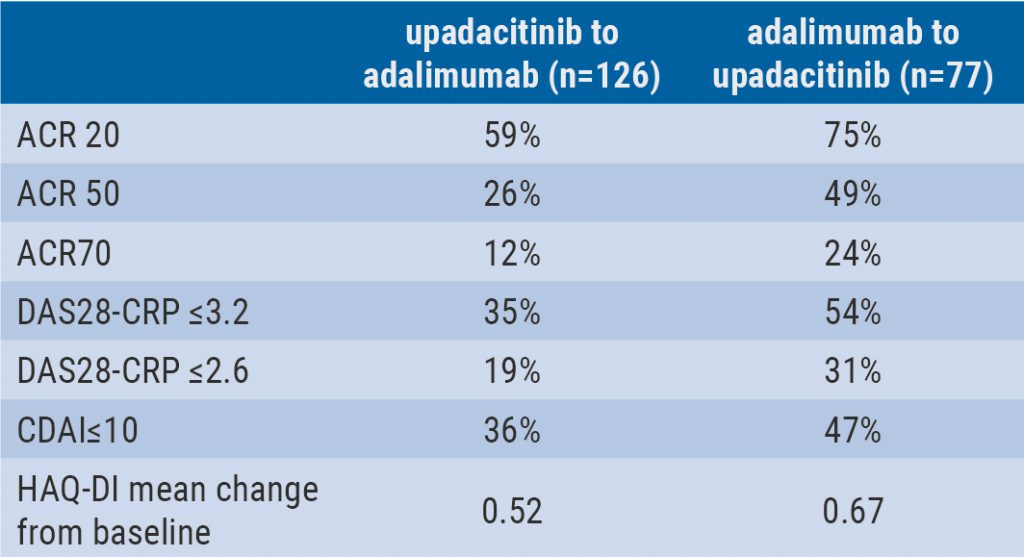
Switching upadacitinib and adalimumab is beneficial in refractory RA
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

