Azathioprine is widely used to treat a variety of illnesses, including systemic lupus erythematosus (SLE) and inflammatory bowel disease (IBD), despite being associated with hematopoietic toxicity.
It's been observed that Black patients discontinue azathioprine for hematopoietic toxicity at a higher rate than white patients.
Dr. Cecilia P. Chung of the Division of Clinical Pharmacology, Vanderbilt University Medical Center, in Nashville, Tennessee, and colleagues hypothesized that this difference was associated with the presence of the rs2814778-CC genotype variant independent of race.
The CC variant is found in roughly half of Americans with recent African ancestry and causes lower white blood cell counts without increased risk of infection, a condition known as benign neutropenia.
The researchers analyzed data on 1,466 new azathioprine users (1,301 white and 165 Black) with indications of lupus, IBD, or other rheumatic conditions.
The rate of stopping azathioprine due to hematopoietic toxicity was nearly three-fold higher in patients with the CC genotype than peers with the TT or TC genotype (hazard ratio, 2.92) and the risk remained significant after adjustment for race and was evident across multiple diseases.
The CC genotype was also independently linked with lower thiopurine doses, the researchers report in Annals of Internal Medicine.
Dr. Chung and colleagues note cell-count monitoring (for example, leukocyte count or absolute neutrophil count) is standard in patients on thiopurine therapy and is meant to help guide decision-making about the safety of continued use and the dose. However, "normal" ranges are primarily derived from patients with European ancestry,
Basing decisions for many Black patients based on low leukocyte counts rather than genotype could lead to unnecessary stopping or inappropriate dosing of azathioprine, they point out.
Based on their results, as well as currently available information for the rs2814778-CC genotypes, the authors recommend that testing for the Duffy-null phenotype be considered in all patients before starting azathioprine or if leukopenia is detected while a patient is taking azathioprine.
They say "next steps for research will be to study whether specific lower leukocyte counts with the rs2814778-CC genotype are associated with greater risks for infection and, if not, whether different leukocyte thresholds are appropriate for discontinuation or dose reduction."
"A second important question to address will be whether patients with the rs2814778-CC genotype taking thiopurines have adverse consequences resulting from under treatment of disease," they add.
Funding for the study was provided by the National Institutes of Health.
SOURCE: https://bit.ly/3mUVBzg Annals of Internal Medicine, online July 20, 2022.
Posted on
Previous Article
« Alcoholic cirrhosis is most common liver transplant indication in young U.S. adults Next Article
ASCO 2022 Highlights Podcast »
« Alcoholic cirrhosis is most common liver transplant indication in young U.S. adults Next Article
ASCO 2022 Highlights Podcast »
Related Articles
November 30, 2021
Guselkumab boosts response in resistant psoriatic arthritis
July 31, 2023
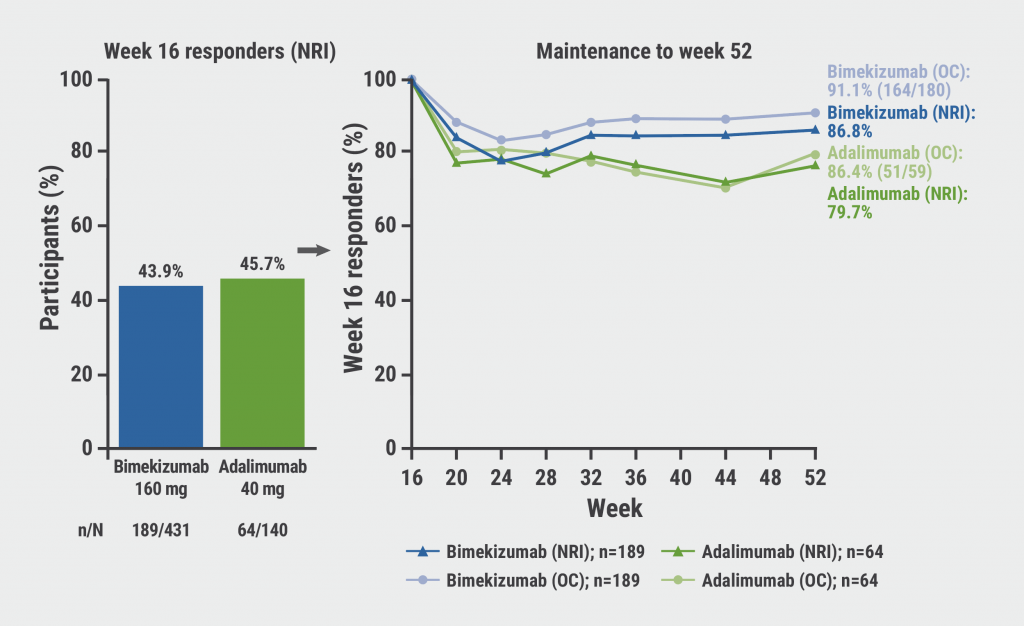
Bimekizumab: high rates of sustained response in PsA
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

