https://doi.org/10.55788/00470d55
CAR T-cell therapy may be an option if immunosuppressive or immunomodulatory therapies fail in SLE. This immunotherapy is successfully used to treat B-cell malignancies and multiple myeloma. A German research group led by Dr Georg Schett (University Hospital Erlangen, Germany) investigated whether CAR T-cell therapy could lead to sustained suppression of SLE-specific autoimmunity and whether it affects long-term vaccination response [1]. The investigators were encouraged by their own previous findings that CD19 CAR T-cell therapy leads to stable, drug-free remission of treatment-resistant SLE [2].
The study consisted of administering a single infusion of 1 million CD19 CAR T cells per kg body weight to 8 patients with treatment-resistant SLE between March 2021 and June 2023. Patients had stopped immunosuppressive treatment before CAR T-cell infusion. SLE disease activity was monitored between 1 and 2 years. Autoantibodies were measured at baseline, 3 months after CAR T-cell therapy, and at the last follow-up.
At the time of analysis (June 2023), 5 participants had a follow-up duration of more than 1 year after treatment with CAR T cells. All 8 patients were in remission and had a Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) score of 0. They were off any immunosuppressive medication. Autoantibodies against dsDNA (4/5), ssDNA (4/5), nucleosomes (5/5), secondary necrotic cells (4/5), and Smith antigen (3/5) disappeared. The one exception was a patient with a nucleosome antibody response.
Vaccination response against measles, mumps, rubella, varicella-zoster, Epstein-Barr, tetanus, and pneumococcus remained stable and robust after treatment. Apparently, antibodies related to vaccination responses predominantly stem from CD19-negative plasma cells, whereas the main source of autoantibodies in SLE may be CD19+ plasmablasts, which are sensitive to CD19 CAR T-cell therapy.
- Schett G, et al. CAR T-cell therapy leads to long-term abrogation of autoimmunity in SLE patients while vaccination responses are maintained. 0607, ACR Convergence 2023, 10–15 November, San Diego, USA.
- Mackensen A, et al. Nat Med. 2022;28(10):2124-2132.
Medical writing support was provided by Michiel Tent.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« IV secukinumab safe and effective for long-term treatment of active PsA Next Article
Romosozumab tops denosumab in glucocorticoid users with high fracture risk »
« IV secukinumab safe and effective for long-term treatment of active PsA Next Article
Romosozumab tops denosumab in glucocorticoid users with high fracture risk »
Table of Contents: ACR 2023
Featured articles
Ixekizumab resolves nail psoriasis better than adalimumab in PsA
IV secukinumab safe and effective for long-term treatment of active PsA
Rheumatoid Arthritis
Short-term glucocorticoid use increases the risk of MACE
Positive efficacy and safety results of novel BlyS/APRIL inhibitor in RA
Baricitinib superior to TNFi in patients with RA who failed csDMARDs
Lupus
Encouraging results of afimetoran in participants with cutaneous lupus
CAR-T cell therapy results in sustained lupus remission
Osteoarthritis
Repeat steroid injection in knee osteoarthritis possibly beneficial
Osteoporosis
Romosozumab tops denosumab in glucocorticoid users with high fracture risk
Psoriatic Arthritis
Ixekizumab resolves nail psoriasis better than adalimumab in PsA
IV secukinumab safe and effective for long-term treatment of active PsA
Apremilast in early oligoarticular PsA: phase 4 study results
Gout
Novel selective URAT1 inhibitor shows promise in gout
Fibrosing rheumatic diseases
Incidence and risk factors for new-onset interstitial lung disease
No need to avoid TNF inhibitors in RA-ILD?
Vasculitis
Reduced-dose glucocorticoids in GPA and MPA increase mortality
Related Articles
March 12, 2021
Primary ovarian insufficiency linked to osteoporosis
August 14, 2020
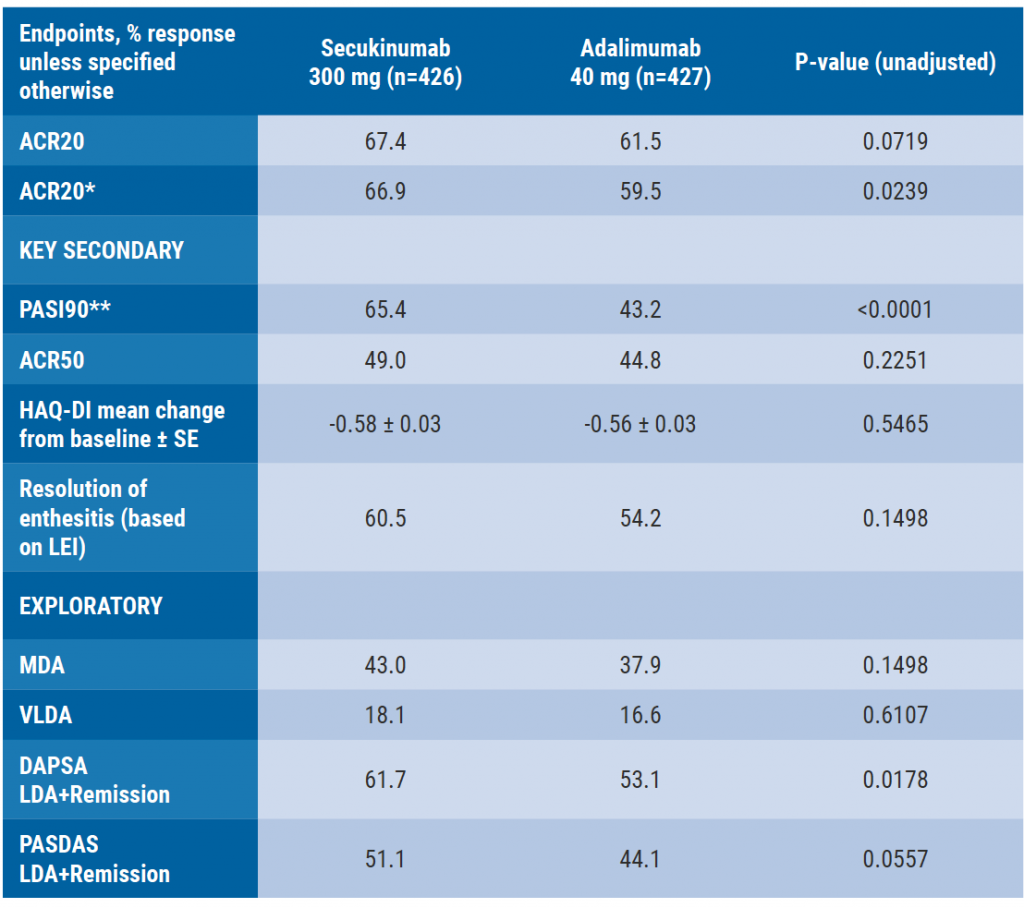
Secukinumab monotherapy as efficient as adalimumab
December 1, 2023
Baricitinib superior to TNFi in patients with RA who failed csDMARDs
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

