The 163 volunteers who got the drug four times per day via an ultrasonic pulsed-delivery nebulizer were covering 21 more meters after 16 weeks of therapy. But for the 163 patients who inhaled placebo, the distance covered by the end of the study had declined by 10 meters (P<0.001).
The results of the company-funded study, known as INCREASE, were released in the New England Journal of Medicine.
"When you add pulmonary hypertension onto interstitial lung disease, it makes the prognosis much worse and functional status declines rapidly," chief author Dr. Aaron Waxman of Brigham and Women's Hospital, in Boston, told Reuters Health by phone.
"By treating the pulmonary hypertension, patients do better, feel better, they get sick less frequently, they can do more because their exercise tolerance improves, and their exacerbations of interstitial lung disease decrease," he said. "So this treatment certainly provides benefit where we really had nothing to offer before."
Dr. Darren Taichman, a deputy editorial at the journal, called the result "exciting" but noted that the improvements "were not accompanied by differences in health-related quality of life."
"Now we need additional, longer-term data to see whether patients will feel better or live longer and to identify which patients and at what costs," Dr. Taichman said.
United Therapeutics has asked the U.S. Food and Drug Administration to expand use of the drug for such patients. A decision is expected in the spring, according to the company.
The scarring of interstitial lung disease produces pulmonary hypertension in an estimated 30,000 patients, the company said in a news release.
Although better treatments have transformed pulmonary arterial hypertension into a disease that can sometimes be managed with drugs, "to date, no such improvements have occurred for patients who have interstitial lung disease-associated pulmonary hypertension," Dr. Taichman said.
Treprostinil is a prostaglandin sold under the brand names Remodulin when it is infused, Orenitram when given by mouth and Tyvaso when inhaled. It is approved for group-1 pulmonary hypertension.
The new study was designed to assess its effectiveness in group-3 patients. All had a forced vital capacity of less than 70% and could walk at least 100 meters in six minutes at baseline.
"I was pretty hopeful we would see these kinds of improvements" when it came to the six-minute walk data, but the team saw more than that, said Dr. Waxman, executive director of the Center for Pulmonary-Heart Diseases at Brigham and Women's Hospital's Heart and Vascular Center.
"From the standpoint of not seeing any worsening of the lung disease and reduced numbers of exacerbations, that's a plus we didn't anticipate," he said.
NT-proBNP levels, a measure of heart failure severity, declined by 15% with the treatment but increased 46% in the placebo group.
The rates of clinical worsening were 22.7% with treprostinil therapy and 33.1% without (P=0.04). Four people died in each treatment group.
The treatment did not seem to significantly affect lung function or oxygenation.
A similar number of patients in each group discontinued therapy, and the rates of serious side effects were 23% with treprostinil versus 26% with placebo.
But those getting the drug reported more cough, throat irritation and oropharyngeal pain.
"I think in real-world practice there may be some patients who may not be able to tolerate the treatment. In some patients it causes some cough issues that, with background lung issues, might not be well tolerated," said Dr. Waxman. "But for the vast majority of patients it will really provide an opportunity for treatment that they didn't have before."
SOURCES: https://bit.ly/38A8tEP and https://bit.ly/35yfRhQ The New England Journal of Medicine, online January 13, 2021.
By Gene Emery
Posted on
Previous Article
« Mitochondria a promising druggable target for Alzheimer’s disease Next Article
Just one drink a day can raise risk of developing atrial fibrillation »
« Mitochondria a promising druggable target for Alzheimer’s disease Next Article
Just one drink a day can raise risk of developing atrial fibrillation »
Related Articles
November 7, 2018
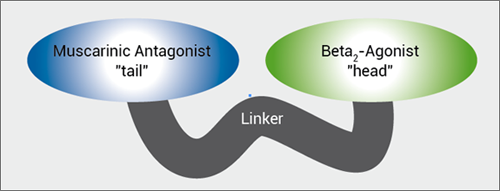
MABA, and novel LAMA
August 17, 2022
Points of interest for radiologists screening for lung cancer
October 30, 2022
Confirmatory mediastinoscopy not needed in resectable NSCLC
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

