https://doi.org/10.55788/2ce7ae0e
Many young breast cancer survivors desire pregnancy. However, standard 5–10 years of adjuvant endocrine therapy compromises conception in women with hormone-positive disease. Although retrospective evidence shows that pregnancy after breast cancer does not worsen the disease outcome, regardless of HR status, women are often discouraged to get pregnant after breast cancer [1].
The POSITIVE trial (NCT02308085) prospectively evaluated outcomes of pregnancy after breast cancer and interruption of endocrine therapy to attempt pregnancy. The study enrolled 518 women (≤42 years) who had at least 18 and no more than 30 months of endocrine therapy for stage I–III HR-positive breast cancer and who desired to become pregnant. After enrolment, women had up to 2 years to attempt pregnancy, conceive, and breastfeed, including a 3-month washout period. Endocrine therapy resumption was strongly recommended after pregnancy to complete the full 5–10 years. The primary endpoint was breast cancer-free interval (BCFI). A cohort of 1,499 patients from the SOFT/TEXT trials were used as external controls [2]. Dr Ann Partridge (Dana-Farber Cancer Institute, MA, USA) presented the results [3].
The median time from breast cancer diagnosis to enrolment was 29 months and the median follow-up from enrolment was 41 months [4]. The cumulative incidence of both BCFI and distant relapse-free interval (DRFI) events at 3 years of follow-up were not statistically different in POSITIVE versus SOFT/TEXT: 8.9% versus 9.2% for BCFI and 4.5% versus 5.8% for DRFI (see Figure). In addition, no difference was observed in BCFI between women in the POSITIVE trial who became pregnant compared with women who did not become pregnant.
Figure: Cumulative incidence of BCFI and DRFI events in POSITIVE versus SOFT/TEXT trials [3]
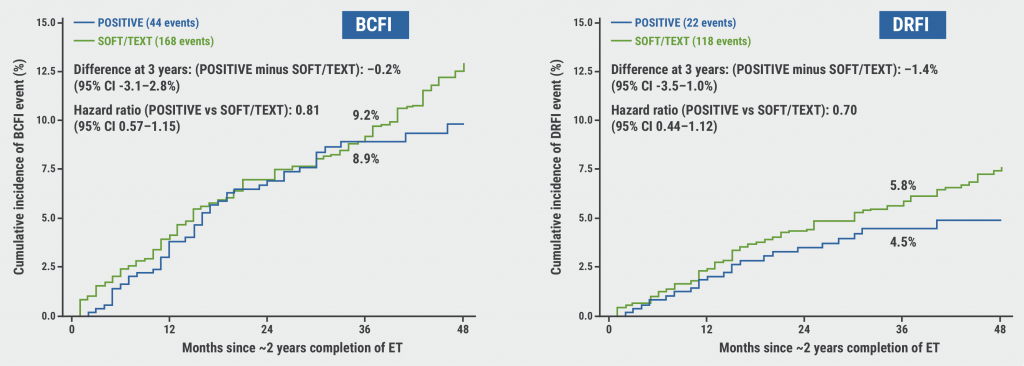
BCFI, breast cancer-free interval; DRFI, distant relapse-free interval; ET, endocrine therapy.
Of the 497 women who were followed for pregnancy status, 368 (74.0%) had at least 1 pregnancy, 317 (63.8%) had at least 1 live birth, with a total of 365 babies (15 sets of twins) born. Birth defects were low (2%) and not clearly associated with treatment exposure. At 48 months, 8% of patients had cancer recurrence or death before resuming endocrine therapy, 76% had resumed endocrine therapy, and 15% had not (yet) resumed endocrine therapy.
Based on these results, Dr Partridge concluded: “Temporary interruption of endocrine therapy to attempt pregnancy among women who desire pregnancy does not impact short-term disease outcomes. These data stress the need to incorporate patient-centred reproductive healthcare in the treatment and follow-up of young women with breast cancer.”
- Lambertini M, et al. J Clin Oncol. 2021;39:3293–3305.
- Sun Z, et al. Breast. 2020;53:1–7.
- Partridge AH, et al. Pregnancy Outcome and Safety of Interrupting Therapy for women with endocrine responsIVE breast cancer. Abstract GS4-09, SABCS 2022, 6–10 December, San Antonio, TX, USA.
- Partridge AH, et al. Breast. 2021;59:327–338.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« ZNF689 deficiency promotes intratumour heterogeneity and resistance to immune checkpoint blockade in TNBC Next Article
Low-dose tamoxifen still prevents recurrence from non-invasive breast cancer »
« ZNF689 deficiency promotes intratumour heterogeneity and resistance to immune checkpoint blockade in TNBC Next Article
Low-dose tamoxifen still prevents recurrence from non-invasive breast cancer »
Table of Contents: SABCS 2022
Featured articles
Miscellaneous
Racial disparity in the tumour microenvironment
Chemo-endocrine therapy worse for cognition than endocrine therapy alone
Early-Stage Breast Cancer
Anti-PD-1/anti-LAG-3 combination highly effective in HER2-negative breast cancer
MammaPrint test predictive for benefit of extended endocrine therapy
HR-positive/HER2-positive Breast Cancer: Trastuzumab-Deruxtecan
Trastuzumab deruxtecan effective in both second-line and neoadjuvant setting
HR-positive/HER2-negative Advanced Metastatic Breast Cancer
Benefit of adjuvant abemaciclib continues to deepen at longer follow-up
First-line ribociclib plus endocrine therapy outperforms combination chemotherapy
Treatment options beyond CDK4/6 inhibition
Triple-Negative Breast Cancer
Baseline CTC count can guide first-line treatment in HR-positive/HER-negative metastatic breast cancer
ZNF689 deficiency promotes intratumour heterogeneity and resistance to immune checkpoint blockade in TNBC
Oestradiol represses anti-tumoural immune response to promote progression of brain metastases
Basic and Translational Research
Resistance to CDK4/6 inhibitors is likely due to expansion of pre-existing resistant clones
Germline pathogenic variants for breast cancer also increase contralateral breast cancer risk
Low-dose tamoxifen still prevents recurrence from non-invasive breast cancer
Endocrine interruption to pursue pregnancy does not impact short-term disease in breast cancer
Related Articles
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

