The study complements the group's earlier work (https://bit.ly/3i2lpV8) showing that 3% of women who are diagnosed with DCIS succumb to breast cancer within 20 years, coauthor Dr. Steven Narod of Women's College Research Institute and the University of Toronto told Reuters Health by email.
"It is generally accepted and communicated to patients that DCIS is not cancer, but a pre-cancer, and that DCIS predisposes to invasive cancer," he said. "Invasive cancer is usually in the form of local recurrence in the same breast, but can be distant recurrence in the lung, liver, brain, bone or lymph nodes."
Preventing local invasion "is a valid goal," he added, "but preventing local invasive recurrence does not prevent distant recurrence. If it did, then women with a bilateral mastectomy should be protected from getting and dying of breast cancer. We showed that women treated for DCIS with bilateral mastectomy had a four-fold greater risk of dying of breast cancer than women without DCIS."
"We propose that DCIS is a bona fide breast cancer in its own right, albeit with a low chance of spreading," he said. "A small node-negative invasive cancer has a 5% mortality. A DCIS has a 3% mortality. These are quantitative, not qualitative, differences."
As reported in JAMA Network Open, Dr. Narod and colleagues analyzed data from SEER on close to 145,000 women diagnosed with DCIS between 1995-2014 (mean age at diagnosis, 57). All underwent surgery, and approximately half received radiation. These women were followed from diagnosis until death from breast cancer or date of the last follow-up (mean follow-up, 9.2 years).
Women in the general population without breast cancer were analyzed as controls. For each woman with DCIS, the team calculated an expected probability of death from breast cancer for a woman in the general population who was cancer-free and with an equal follow-up time.
During follow-up, 1,540 deaths from breast cancer occurred among those diagnosed with DCIS. In addition, there were 4,502 (3.1%) ipsilateral invasive recurrences, resulting in a 20-year actuarial risk of 13.9%.
Similarly, there were 5,527 (3.8%) contralateral invasive events, resulting in a 20-year actuarial risk of 11.3%. Overall, the 20-year actuarial risk of breast cancer death among women with DCIS was 3.3%.
Based on national incidence and case-fatality rates, the expected number of deaths from breast cancer in the control group was 458. The standardized mortality ratio for death from breast cancer given a diagnosis of DCIS was 3.36, and the elevated risk of death persisted more than 15 years after diagnosis.
Dr. Andrea Porpiglia, a surgical oncologist at Fox Chase Cancer Center in Philadelphia, told Reuters Health by email she has "reservations" about the findings.
"This was an observational study and I am cautious about generalizing these results to...how we manage our patients with DCIS," she said. "Furthermore, since this is a retrospective study, it has an inherent selection bias."
"The study excluded untreated patients with DCIS and patients who were treated did very well," she noted, with only a 1% mortality rate (1,540 deaths among 144,524 women diagnosed).
"Another concern is the limited follow up," she said. "In addition, the study did not comment on women receiving adjuvant endocrine therapy. According to the National Comprehensive Cancer Guidelines, endocrine therapy should be considered for patients who underwent breast conservation therapy (lumpectomy and radiation therapy) or surgery alone."
"Lastly, there have been four randomized phase III studies demonstrating a 10% absolute decrease in ipsilateral breast cancer recurrence when patients received radiation in addition to lumpectomy," she added. "However, in this study, 67% of patients had a lumpectomy but only 47% had radiation therapy. There is no (mention of) why 13% of patients did not receive radiation."
By Marilynn Larkin
SOURCE: https://bit.ly/3j0Q8TT JAMA Network Open, online September 16, 2020.
Posted on
Previous Article
« Arthroscopic partial meniscectomy tied to radiographic knee osteoarthritis Next Article
Expert-center referral after pancreatectomy does not improve outcomes »
« Arthroscopic partial meniscectomy tied to radiographic knee osteoarthritis Next Article
Expert-center referral after pancreatectomy does not improve outcomes »
Related Articles
January 31, 2022
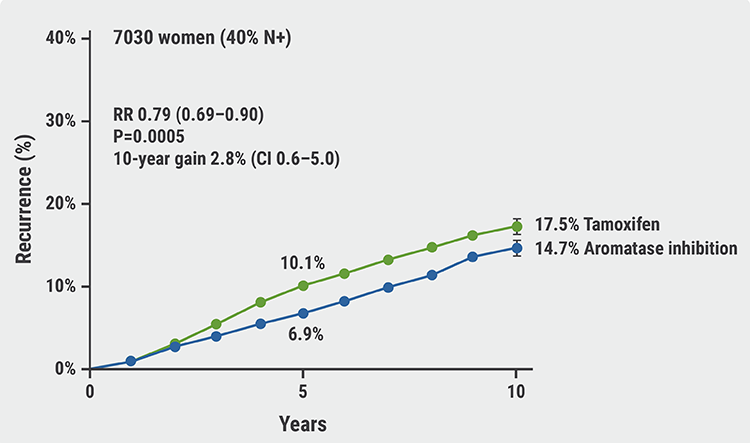
Aromatase inhibitors outperform tamoxifen in premenopausal women
June 16, 2021
Breast cancer treatment decreases risk of dementia
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

