In Europe, cenobamate is approved for the adjunctive treatment of focal-onset seizures with or without secondary generalisation, in adult patients who have not been adequately controlled despite a history of treatment with at least 2 anti-epileptic drugs. In C013 (NCT01397968) [3] and C017 (NCT01866111) [4], 2 international, double-blind, placebo-controlled trials with open-label extensions (OLE), efficacy and safety were assessed. A pooled post-hoc analysis established time to onset of efficacy during titration [1].
In C013, participants were randomised to placebo (n=108) or cenobamate 200 mg/day (n=113). Cenobamate was titrated by 50 mg/day every 2 weeks until the maintenance dose of 200 mg/day was reached. Patients in the cenobamate group had significant reductions in median percentage seizure frequency of -26.7% versus -15.1% in the placebo group (P<0.05), starting as early as in the first 1–2 weeks of titration at 50 mg/day.
In C017, participants were randomised to placebo (n=106), cenobamate 100 mg/day (n=108), 200 mg/day (n=109), or 400 mg/day (n=111). The initial starting dose of 100 mg/day was reduced to 50 mg/day, after which the titration rate to target dose was slowed to improve tolerability. As in C013, participants had significant reductions in median percentage seizure frequency (-36.4%) versus placebo (-20.0%; P<0.05), starting in the first week of titration at 50 mg/day.
In both studies, sustained significant decreases in seizure frequency with cenobamate versus placebo were seen throughout the 6-week titration period. The median reduction in seizure frequency was progressively higher with increasing cenobamate doses of 100, 200, and 400 mg/day.
In a second pooled ad-hoc analysis, time to onset, duration, and severity of the most common AEs were assessed in 3 studies: C013, C017, and the large international open-label safety study C021 (NCT02535091) [2,5]. In C021 (n=1,339) cenobamate titration started at a lower dose, which was also up-titrated slower than in C013/C017 (“start low, go slow”). Patients initiated cenobamate at 12.5 mg/day for 2 weeks, followed by 25 mg/day for 2 weeks and 50 mg/day for 2 weeks; the dose was then increased by 50 mg/day at 2-week intervals to the target dose of 200 mg/day. Maximum dose was 400 mg/day. The analysis focused on the most common AEs: somnolence, dizziness, and fatigue.
AEs emerged throughout the double-blind period and OLE, mostly during titration. In C021, AEs peaked when dose reached 50 mg/day. Median duration in days during the double-blind period shows AEs were generally self-limited in duration:
- somnolence: cenobamate 32%, placebo 22%;
- dizziness: cenobamate 11%, placebo 8%;
- fatigue: cenobamate 34%, placebo 20.5%.
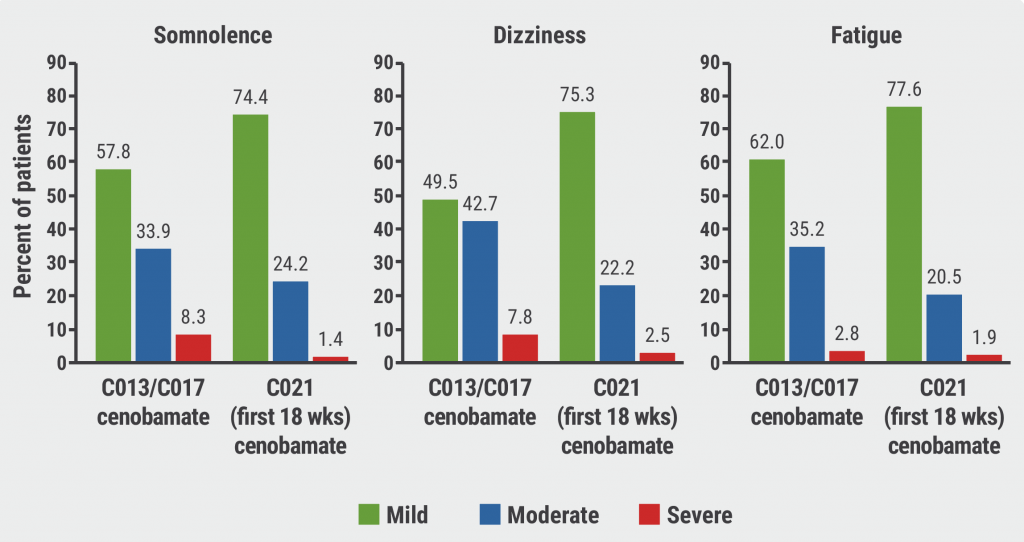
AEs in the double-blind period of C013 and C017 were primarily mild or moderate, with few severe AEs. In C021, AEs were more often mild and fewer were moderate and severe (see Figure). The authors concluded that slower titration, using the currently recommended schedule, reduced severity of the most common AEs.
Figure: Severity of most common adverse events in C013, C017, and C021 [5]
- Steinhoff BJ, et al. Cenobamate as adjunctive therapy in adults with uncontrolled focal seizures: time to onset of efficacy during titration. EPR-307, EAN 2021 Virtual Congress, 19–22 June.
- Steinhoff BJ, et al. Safety of adjunctive cenobamate in adults with uncontrolled focal seizures: time to onset, duration, and severity of Aes. OPR-153, EAN 2021 Virtual Congress, 19–22 June.
- Chung SS, et al. Neurology. 2020;94(22):e2311-22.
- Krauss GL, et al. Lancet Neurol. 2020;19(1):38-48.
- Sperling MR, et al. Epilepsia. 2020;61(6):1099-108.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Promising diagnostic accuracy of plasma GFAP Next Article
Stroke with covert brain infarction indicates high vascular risk »
« Promising diagnostic accuracy of plasma GFAP Next Article
Stroke with covert brain infarction indicates high vascular risk »
Table of Contents: EAN 2021
Featured articles
Letter from the Editor
COVID-19
First evidence of brainstem involvement in COVID-19
Cognitive/behavioural alterations persistent after COVID-19
Neural base of persistent hyposmia after COVID-19
Neurological symptoms and complications of COVID-19 affect outcomes
Cerebrovascular Disease
Intracerebral haemorrhage only slightly increases mortality in COVID-19 patients
Stroke with covert brain infarction indicates high vascular risk
Expanding precision medicine to stroke care
Dexamethasone not indicated for chronic subdural haematoma
Cognitive Impairment and Dementia
Severe outcomes of COVID-19 in patients with dementia
Promising diagnostic accuracy of plasma GFAP
Sex modulates effect of cognitive reserve on subjective cognitive decline
Hypersensitivity to uncertainty in subjective cognitive decline
Epilepsy
Minimally invasive device to detect focal seizure activity
‘Mozart effect’ in epilepsy: why Mozart tops Haydn
Migraine and Headache
Factors associated with decreased migraine attack risk
Pregnant migraine patients at higher risk of complications
Occipital nerve stimulation in drug-resistant cluster headache
Rhythmicity in primary headache disorders
Multiple Sclerosis and NMOSD
Typing behaviour to remotely monitor clinical MS status
Alemtuzumab in treatment-naïve patients with aggressive MS
No higher early MS relapse frequency after stopping ponesimod
Good long-term safety and efficacy of inebilizumab in NMOSD
Neuromuscular Disorders
Inability to recognise disgust as first cognitive symptom of ALS
Pathogenic T-cell signature identified in myasthenia gravis
Parkinson’s Disease
Levodopa-carbidopa intestinal gel in patients with advanced PD
New Frontier – Navigated Transcranial Ultrasound
Exploring the possibilities
Related Articles
August 18, 2021
Stroke with covert brain infarction indicates high vascular risk
August 18, 2021
Alemtuzumab in treatment-naïve patients with aggressive MS
August 18, 2021
Machine-learning method accurately classifies patients with MS
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

