"While the role of cholesterol synthesis has been the focus of much attention in relation to its risk for cardiovascular disease and dementia, much less is known about the relationship between cholesterol catabolism - i.e., breakdown - and dementia," lead study author Dr. Vijay Varma of the U.S. National Institute on Aging (NIA) told Reuters Health by email.
"The main breakdown products of cholesterol are BAs that help in absorbing fats from the gut," he said. "However, recent studies are also showing that they may have important roles to play as signaling molecules in the brain and in the regulation of blood sugar levels."
Principal author Dr. Madhav Thambisetty, also of the NIA, noted, "Our study shows that the levels of BAs in blood are related to measures of dementia such as brain amyloid and atrophy. Older individuals prescribed medications that lower BA levels to reduce blood cholesterol appear to have a slightly greater risk of vascular dementia."
"It was surprising to see that this effect was only observed in males," he added.
As reported in PLoS Medicine, the team used a three-step study design to examine the role of the primary BAs - cholic acid (CA) and chenodeoxycholic acid (CDCA) - as well as their principal biosynthetic precursor, 7alpha-hydroxycholesterol, in dementia using the Baltimore Longitudinal Study of Aging (BLSA), the Alzheimer's Disease Neuroimaging Initiative (ADNI) and other large data sets.
First, they tested whether serum markers of cholesterol catabolism were associated with brain amyloid accumulation, white matter lesions, and brain atrophy. They found a modest sex-specific effect indicating that lower serum concentrations of CA and CDCA were associated with faster brain atrophy.
Next, they tested whether exposure to BA sequestrants was associated with risk of dementia, analyzing more than 26,000 patients from general practice clinics in the United Kingdom. They found that BA sequestrant users (3,208 with two or more prescriptions) had altered dementia risk compared to those on non-statin lipid modifying therapies (LMT users; 23,483 with two or more prescriptions).
While BA sequestrant use was not significantly associated with risk of all-cause dementia (hazard ratio, 1.03) or its subtypes, a significant difference was seen between the risk of vascular dementia (VaD) in men compared to women, as well as a significant dose-response relationship between BA sequestrant use and risk of VaD in men.
Finally, they examined 29 autopsy samples from the BLSA to determine whether people with Alzheimer's disease tend to have altered levels of bile acids in their brains. They found that CA and CDCA were detectable in the samples and were marginally higher in AD samples compared to controls. In another database of autopsy samples, Religious Orders Study and Memory and Aging Project, they found sex-specific differences in altered neuronal gene expression of BA receptors in AD.
Study limitations included relatively small numbers of autopsy samples, small sample sizes in the BLSA cohort, and likely inaccuracies in the clinical diagnosis of dementia subtypes in primary care, underscoring the need for further study.
Dr. Thambisetty added, "In the ongoing Drug Repurposing for Effective Alzheimer's Medicines (DREAM) study (https://bit.ly/35cx3Jg), we are testing whether some commonly used drugs for diseases such as high blood pressure, asthma, and diabetes that are known to alter BA signaling may protect against AD."
Dr. Mark Forman, Senior Director of Drug Development at the Alzheimer's Drug Discovery Foundation in New York City, commented in an email to Reuters Health, "We agree with the authors that their findings warrant further study."
"We have long known there is an association between high cholesterol and an increased risk of Alzheimer's and vascular dementia," he said, "but since cholesterol doesn't cross the blood-brain barrier and enter the brain, the question has been, why?"
"While this study provides important evidence about possible connections between cholesterol breakdown and higher amyloid levels and other abnormalities in the brain," he said, "more validation studies and clinical research are needed before clinicians change anything about how they treat cholesterol."
SOURCE: https://bit.ly/35cnZUF PLoS Medicine, online May 27, 2021.
By Marilynn Larkin
Posted on
Previous Article
« Should the recurrence score for downstaging breast cancer be expanded? Next Article
Prevalence of breast-cancer-susceptibility genes similar in Black and white women »
« Should the recurrence score for downstaging breast cancer be expanded? Next Article
Prevalence of breast-cancer-susceptibility genes similar in Black and white women »
Related Articles
December 4, 2023
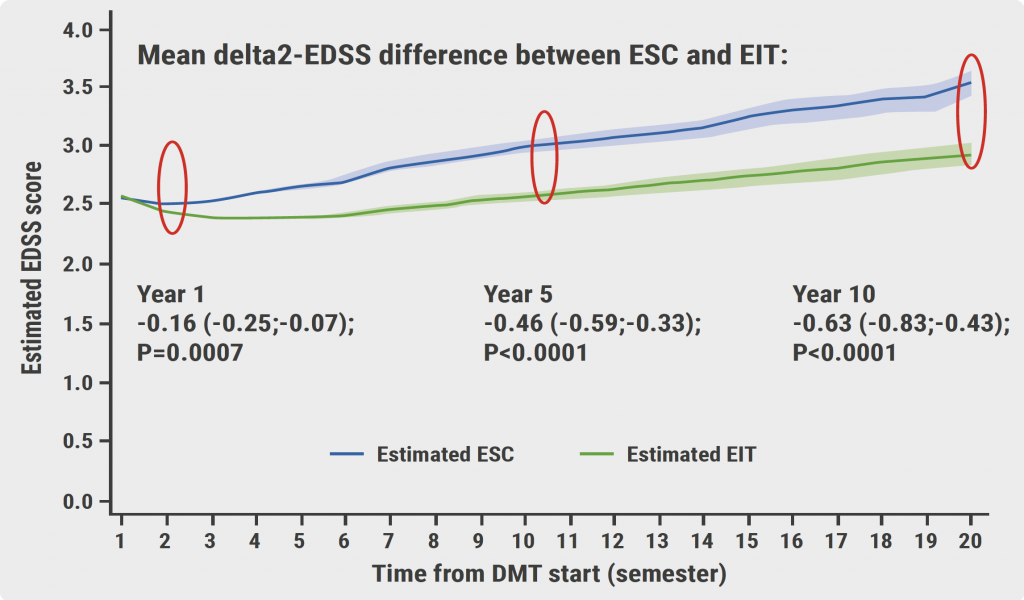
Early intensive treatment enhances long-term clinical outcomes
November 8, 2019
Determinants of outcomes for natalizumab-associated PML
November 8, 2019
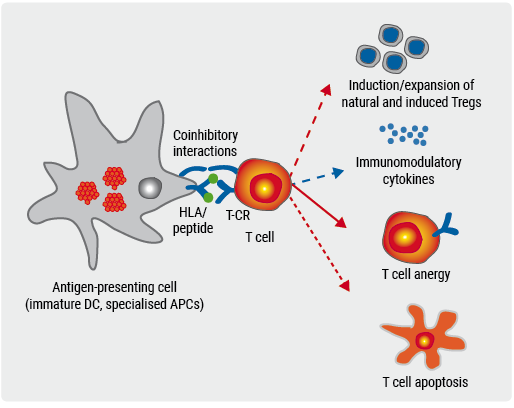
Late-breaking: Myelin-peptide coupled red blood cells
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

