https://doi.org/10.55788/de1867a4
“Many newly diagnosed patients with CML do not achieve an optimal response with standard TKIs,” opened Prof. Andreas Hochhaus (Jena University Hospital, Germany) [1]. “Moreover, long-term use of TKIs has been linked to renal failure, pleural effusion, and other adverse events.” The phase 3 ASC4FIRST trial (NCT04971226) randomised 405 participants with untreated CML in the chronic phase 1:1 to the new-generation BCR::ABL1 TKI inhibitor asciminib or an investigator-selected standard-of-care TKI.
Treatment with the first-generation TKI imatinib, or one of the second-generation TKIs bosutinib, dasatinib, or nilotinib was permitted for ≤ 2 weeks before randomisation. Prof. Hochhaus presented the results and noted that randomisation was stratified by pre-randomisation TKI selection and the European Long-Term Survival (ELTS) risk category. The primary endpoints were major molecular response (MMR) at week 48 and MMR within the imatinib stratum.
The first primary endpoint was met: 67.7% of the participants in the asciminib and 49.0% in the control arm reached an MMR at week 48 (Δ 18.9; 95% CI 9.6–28.8; P<0.001). In addition, MR4.5 (BCR::ABL1 ≤0.0032%) was seen in 16.9% of participants in the asciminib arm compared with 8.8% in the control arm (see Figure). In the imatinib stratum, the MMR rates were 69.3% and 40.2%, in favour of the asciminib arm, meeting the second primary endpoint (Δ 29.6; 95% CI 16.9–42.2; P<0.001). Of note, the difference in MMR between the asciminib arm (66.0%) and control arm (57.8%) within the second-generation TKI stratum was less pronounced (95% CI -5.1 to 21.5).
Figure: More participants achieved early/deep molecular responses with asciminib as compared with investigator-selected TKIs [1]
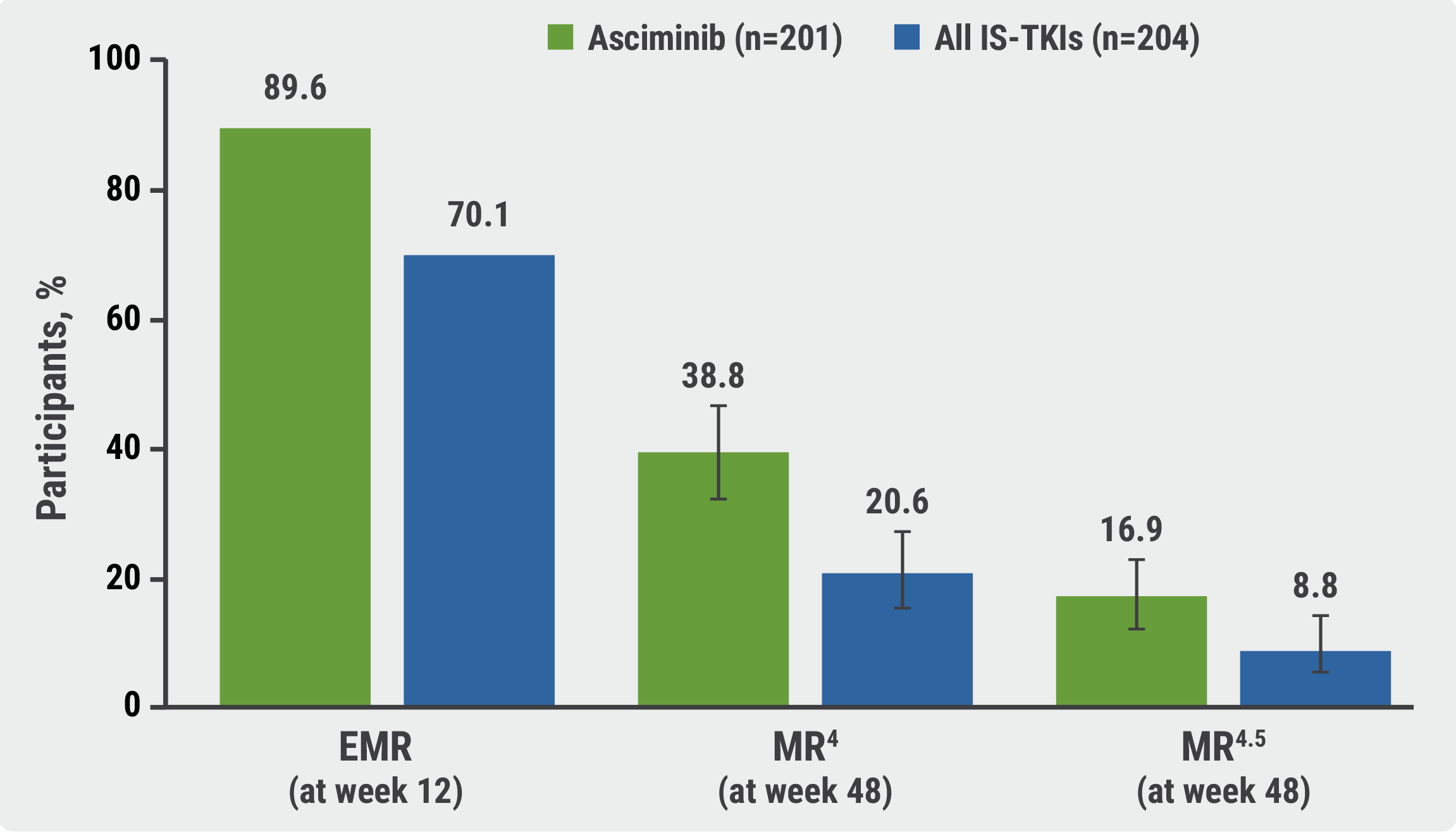
EMR, early molecular response; IS, investigator-selected; MR, molecular response; TKIs, tyrosine kinase inhibitors.
Fewer grade ≥3 adverse events were documented in the asciminib arm (38.0%) compared with participants who received imatinib (44.4%) or second-generation TKIs (54.9%). Similarly, the adverse events-related treatment discontinuation rate was lower (4.5% vs 11.1% and 9.8%) on asciminib. “We saw less neutropenia, anaemia, and lymphopenia with asciminib,” added Prof. Hochhaus. Also, diarrhoea, nausea, and muscle spasms were less common in the asciminib arm.
Asciminib displayed a favourable safety profile and provided better efficacy outcomes than first-line standard-of-care TKIs in newly diagnosed participants with CML in the chronic phase.
- Hochhaus A, et al. Asciminib provides superior efficacy and excellent safety and tolerability vs tyrosine kinase inhibitors in newly diagnosed chronic myeloid leukemia in the pivotal ASC4FIRST study. S103, EHA congress 2024, 13–16 June, Madrid, Spain.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« AUGMENT-101: Revumenib trial in KMT2Ar leukaemia stopped early for efficacy Next Article
APOLLO: ATRA plus ATO meets expectations in high-risk APL »
« AUGMENT-101: Revumenib trial in KMT2Ar leukaemia stopped early for efficacy Next Article
APOLLO: ATRA plus ATO meets expectations in high-risk APL »
Table of Contents: EHA 2024
Featured articles
Meet the Expert: Prof. C. Ola Landgren discusses MRD as a key endpoint in haematological cancer trials
Multiple Myeloma
Isa-VRd proves its value in newly diagnosed MM in the IMROZ trial
PERSEUS: High MRD negativity rates with D-VRd and consolidation therapy and D-R maintenance in MM
Post-intensification data confirm superiority of quadruple therapy in MM
Promising phase 1 results for novel CAR T-cell therapy in MM
DREAMM 8: Belantamab mafodotin offers hope for patients with RRMM
Leukaemia
PhALLCON: Third-generation TKI superior to first-generation TKI in Ph+ ALL
APOLLO: ATRA plus ATO meets expectations in high-risk APL
Excellent phase 3 results for asciminib in chronic myeloid leukaemia
AUGMENT-101: Revumenib trial in KMT2Ar leukaemia stopped early for efficacy
FLAG-Ida plus venetoclax induces high MRD-negativity rates in AML
CD40/CD47 inhibitor shows promise in high-risk MDS and AML
ENHANCE: Magrolimab does not ameliorate health outcomes in high-risk MDS
Can MRD-guided azacitidine treatment improve outcomes in AML and MDS?
Can WGTS replace standard-of-care diagnostics in AML?
Non-malignant Haematology
ENERGIZE: Mitapivat meets primary efficacy endpoint in thalassaemia
Sovleplenib delivers durable responses and QoL improvements in primary ITP
Avatrombopag successful in children with chronic ITP
RUBY: Promising data for first AsCas12a gene-editing therapy in sickle cell disease
Encouraging data for ELA026 to treat secondary haemophagocytic lymphohistiocytosis
Myelofibrosis
Navitoclax plus ruxolitinib leads to spleen volume reductions in myelofibrosis
Is pelabresib plus ruxolitinib the paradigm-shifting combo therapy for myelofibrosis?
Lymphoma
The landscape of TP53 mutations and their prognostic impact in CLL
Can golcadomide plus R-CHOP become the first-line standard of care in high-risk BCL?
High survival rates following atezolizumab consolidation in DLBCL
First results for zanubrutinib plus venetoclax in del(17p)/TP53-mutated CLL/SLL
EPCORE CLL-1: Promising data for epcoritamab in high-risk Richter’s transformation
Updates from the EBMT Lymphoma Working Group: outcomes after allo- and auto-SCT for T-cell lymphoma subtypes
ECHO: Can we expect a novel standard of care in newly diagnosed MCL?
Clinically meaningful outcomes for mosunetuzumab across follicular lymphoma subgroups
Related Articles
December 11, 2024
ATALANTA-1: Promising data for novel CAR T-cell therapy
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

