https://doi.org/10.55788/0c4b13e8
CAR T-related haematological toxicity is a frequently occurring phenomenon, and prolonged cytopenia and complications due to infections contribute to the toxicity burden of CD19-directed CAR T therapy [1]. “The CAR-Hematotox score predicts the risk for prolonged neutropenia, severe infections, and poor treatment outcomes after CD19 CAR T-cell therapy,” said Dr Kai Rejeski (LMU Munich, Germany) [1,2]. The use of this tool in patients with relapsed/refractory MCL undergoing CD19 CAR T-cell therapy has not yet been established. Therefore, the current international, multicentre, retrospective study analysed the applicability of the CAR-Hematotox score in 103 patients with relapsed/refractory MCL receiving brexu-cel.
At baseline, high CAR-Hematotox scores (HT-high) were related to aggressive disease biology, increased bone marrow infiltration, a higher number of prior treatments, and increased disease activity. It was demonstrated that patients with HT-high had higher risk for haematologic toxicity than patients with HT-low: neutropenia (median 14 vs 6 days; P<0.001); aplastic phenotype (47% vs 0%; P<0.001); severe anaemia (45% vs 11%; P<0.0001); profound (85% vs 46%; P<0.0001) or prolonged cytopenia (66% vs 30%; P<0.0004). Furthermore, severe infections were more common in HT-high patients than in HT-low patients (30% vs 5%; P=0.001), mostly driven by an increase in bacterial infections (28% vs 5%; P=0.002). Finally, after 720 days of follow-up, HT-high scores were associated with poorer progression-free survival (38% vs 79%; P<0.0001) and overall survival (52% vs 90%; P=0.00016).
In summary, HT-high patients had an increased risk to develop severe haematotoxicity and infectious complications and had a reduced progression-free and overall survival compared with HT-low patients. Dr Rejeski commented that a risk stratification for haematological toxicity and infections should be performed before lymphodepletion in order to initiate prophylactic strategies in time.
- Rejeski K, et al. Blood. 2021;138(24):2499–2513.
- Rejeski K, et al. The CAR-Hematotox Score Identifies Patients at High Risk for Hematological Toxicity, Infections and Poor Clinical Outcomes Following BrexucabtageneAutoleucel in Relapsed/Refractory Mantle Cell Lymphoma. Abstract 264, ASH 64th Annual Meeting, 10–13 December 2022, New Orleans, LA, USA.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« Talquetamab further investigated in heavily pre-treated MM after promising phase 2 data Next Article
Excellent results for AFM13-complexed NK cells in CD30-positive lymphoma »
« Talquetamab further investigated in heavily pre-treated MM after promising phase 2 data Next Article
Excellent results for AFM13-complexed NK cells in CD30-positive lymphoma »
Table of Contents: ASH 2022
Featured articles
Acute Lymphoblastic Leukaemia
Blinatumomab candidate for standard-of-care in newly diagnosed B-ALL
High-dose methotrexate or standard interim maintenance in young patients with ALL?
Acute Myeloid Leukaemia
Excellent results for triplet regimen in FLT3-mutated AML
MRD by qPCR prognostic of outcomes in venetoclax-treated NPM1-mutated AML
Promising results for triplet therapy with magrolimab in AML
Should we use intensive chemotherapy prior to allo-HCT in relapsed/refractory AML?
Chronic Leukaemia
Zanubrutinib wins battle of BTK inhibitors in relapsed or refractory CLL/SLL
Ibrutinib plus venetoclax displays long-term benefits in CLL
Multiple Myeloma
Talquetamab further investigated in heavily pre-treated MM after promising phase 2 data
Promising results of elranatamab for MM in phase 2 MagnetisMM-3 trial
Deep and durable responses for quadruple therapy in smouldering MM
Ultra-sensitive MRD assessment in MM with BloodFlow
CAR-Hematotox score proves useful in relapsed/refractory MM
Head-to-head: VMP versus Rd in transplant-ineligible MM
Lymphoma
Ibrutinib added to ASCT improves clinical outcomes in mantle cell lymphoma
High-dose chemotherapy plus ASCT superior to standard immuno-chemotherapy in primary CNS lymphoma
Odronextamab has considerable anti-tumour effects in relapsed/refractory diffuse large B-cell lymphoma and follicular lymphoma
Excellent results for AFM13-complexed NK cells in CD30-positive lymphoma
CAR-Hematotox score predicts toxicity, infections, and clinical outcomes in MCL
Myeloproliferative Neoplasms
Efgartigimod successful in immune thrombocytopenia
INCA033989: novel investigational agent for CALR-mutated MPN
Ruxolitinib mediates clonal evolution of RAS pathway mutations in MPN
Immune Thrombocytopenia
Long-term risk for haematologic disease in persistent, isolated mild thrombocytopenia
Various Topics
C1 inhibitor deficiency linked to thrombosis
Durable responses to gene therapy in haemophilia A
Long-term benefits from beti-cel in transfusion-dependent β-thalassaemia
Neutrodiet: non-restricted diet is the preferred option after SCT
Iptacopan offers solution for patients with PNH and residual anaemia after standard-of-care
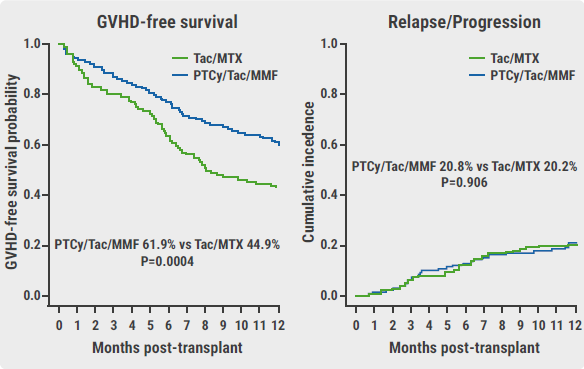
Novel therapy may replace standard-of-care prophylaxis for GVHD
LMWH does not result in higher live birth rates in women with inherited thrombophilia
Related Articles
February 20, 2023
C1 inhibitor deficiency linked to thrombosis
February 20, 2023
Novel therapy may replace standard-of-care prophylaxis for GVHD
February 20, 2023
Neutrodiet: non-restricted diet is the preferred option after SCT
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

