
In patients with relapsed/refractory large B-cell lymphoma (R/R LBCL), infusion of CD22-directed CAR T-cell therapy (CAR22) was found to be safe and well-tolerated at dose level 1 (DL1, 1x106 CAR+ cells/kg) [1]. The manufacturing of CAR22 was uniformly successful. This was found in an ongoing single-institution phase 1 dose-escalation clinical trial (NCT04088890) from Stanford University School of Medicine, in California, USA.
CD19-directed CAR T-cell therapy (CAR19) has achieved durable complete response (CR) rates of 30-40% in patients with R/R LBCL [2-4]. Unfortunately, after failure of CAR19, these patients have a poor prognosis, with an objective response rate (ORR) of 29% to conventional salvage therapies, a median progression-free survival (PFS) of 1.8 months, and a median overall survival (OS) of 6 months [5].
Approximately 30% of the patients who experienced post-CAR19 relapses had CD19 loss or decreased expression [2,5]. “This suggests that antigen escape represents an important mechanism of relapse in lymphoma,” Dr Matthew J. Frank (Stanford University School of Medicine, USA) argued. “Given the poor prognosis of patients after relapsing to CAR19 therapies, there is an urgent unmet need for this patient population.”
Targeting CD22
CD22 is a sialic acid-binding immunoglobulin-like lectin (Siglec-2) restricted to the B-cell lineage [6]. CD22 is detectable on the surface of malignant B cells in 95% of B-cell acute lymphoblastic leukaemia (B-ALL) and LBCL [6-8], “making it an excellent target for CAR T-cell therapies,” according to Dr Frank.
Treatment with a CD22-directed chimeric antigen receptor (CAR) T-cell therapy resulted in a 70% CR rate in 58 paediatric patients with heavily pre-treated ALL [9]. Based on these encouraging results, Dr Frank and colleagues evaluated CAR22 in adult patients with R/R LBCL (n=21; median age 64), focusing on those with CAR19-refractory disease.
Safety and efficacy findings
CAR22 was successfully manufactured in 100% of the patients using a close CliniMACS Prodigy system. The median vein-to-vein time, defined as the time between apheresis and infusion, was 17 days.
The safety profile of CAR22 appears comparable with CAR19. 1 case of grade 3 cytokine release syndrome (CRS) occurred (none at DL1), and no cases of high-grade immune effector cell-associated neurotoxicity syndrome (ICANS) were reported at any dose level. The 5 cases of macrophage activation syndrome (MAS), an emerging CAR22-related hyperinflammatory toxicity, and grade 3 infections were manageable.
A single infusion of CAR22 produced high response rates in heavily pre-treated patients with LBCL. The best ORR at Day 28 was 79% and the best CR rate was 58%. . Notably, low CD22 expression appears to be a mechanism of resistance to CAR22.
- Frank MJ, et al. CD22-CAR T-Cell Therapy Mediates High Durable Remission Rates in Adults with Large B-Cell Lymphoma Who Have Relapsed after CD19-CAR T-Cell Therapy. Abstract 741, ASH 2021 Annual Meeting, 11-14 Dec.
- Neelapu SS, et al. Blood 2019;134(suppl_1):203.
- Schuster SJ, et al. Blood 2018;132(suppl_1):1684.
- Abramson JS, et al. Lancet. 2020;396:839–852.
- Spiegel JY, et al. Blood. 2021;137:1832–1835.
- Boyd SD, et al. Appl Immunohistochem Mol Morphol. 2013;21:116–31.
- Shah NN, et al. Pediatr Blood & Cancer. 2015;62:964–9.
- Majzner RG, et al. Cancer Discov. 2020 May;10(5):702–723.
- Shah NN, et al. J Clin Oncol. 2020;38:1938–1950.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« MajesTEC-1: Teclistamab efficacious in heavily pre-treated MM Next Article
GRIFFIN: Sustained responses of daratumumab plus RVd in MM »
« MajesTEC-1: Teclistamab efficacious in heavily pre-treated MM Next Article
GRIFFIN: Sustained responses of daratumumab plus RVd in MM »
Table of Contents: ASH 2021 Focus on CAR T-Cell Therapy
Featured articles
Axi-cel improved event-free survival in relapsed/refractory large B-cell lymphoma
CAR T-cell Therapy
Most re-hospitalisations within first month from CAR T-cell infusion
CD22-directed CAR T-cell therapy safe and well-tolerated in R/R LBCL
High rate of rapid and complete responses with axi-cel in high-risk large B-cell lymphoma
Novel anti-CD19 plus lenalidomide prolonged survival in R/R DLBCL
Liso-cel superior to standard-of-care as second-line therapy in large B-cell lymphoma
CIRS is predictive of outcomes in CAR T-cell recipients with R/R DLBCL
Axi-cel more effective but tisa-cel less toxic in large B-cell lymphoma
Axi-cel improved event-free survival in relapsed/refractory large B-cell lymphoma
Comparable outcomes with second-line tisa-cel versus standard-of-care for relapsed/refractory aggressive NHL
Improved QoL with axi-cel versus standard-of-care in R/R LBCL
Related Articles
February 18, 2021
More complicated course of COVID-19 in leukaemia patients
August 28, 2020
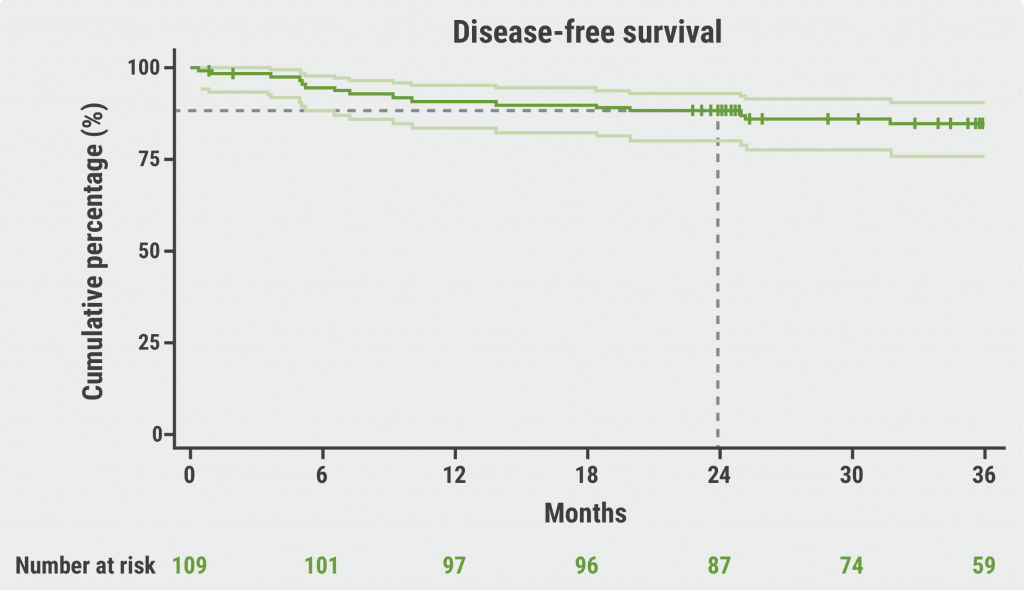
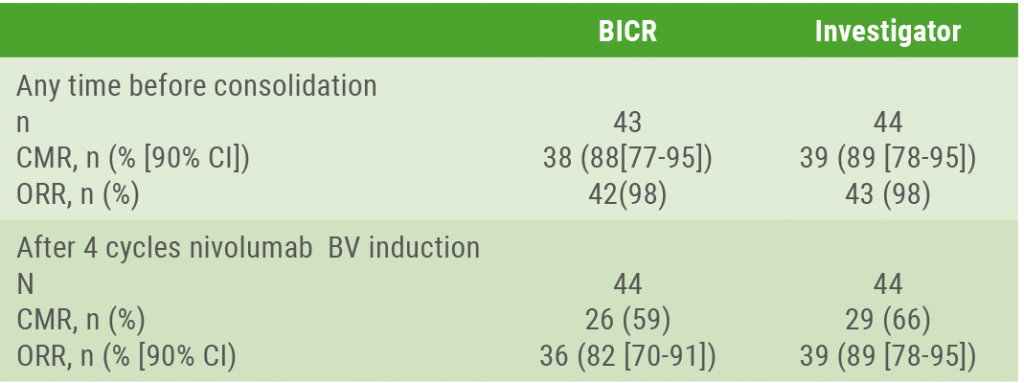
Nivolumab/brentuximab vedotin in R/R HL: good CMR rates
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

