Risankizumab is an IL-23 inhibitor under investigation for the treatment of patients with CD.
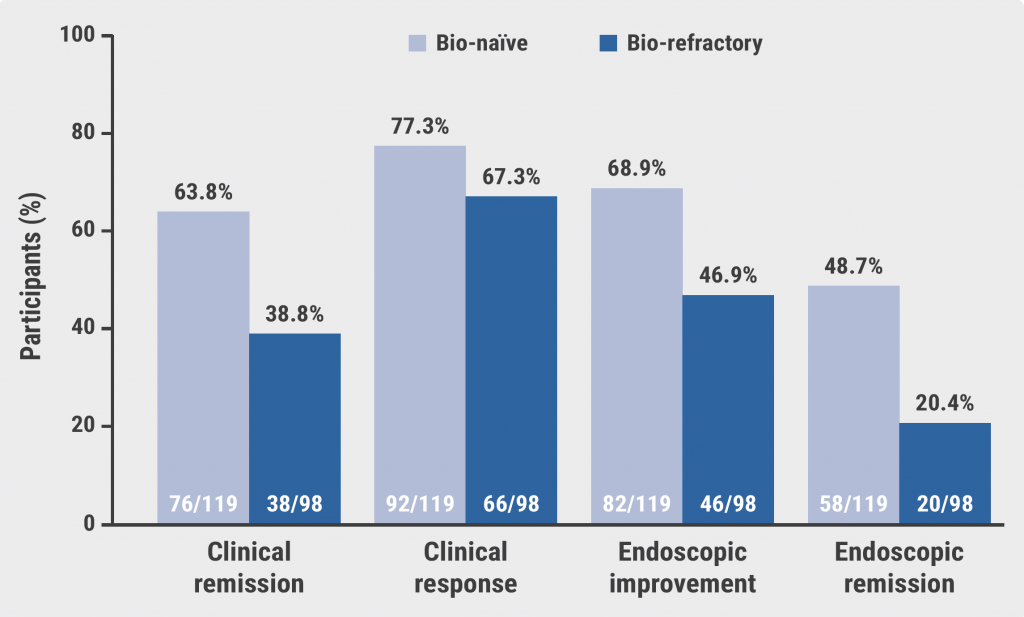
Although several phase 3 trials have demonstrated the safety and efficacy of risankizumab as intravenous induction therapy and subcutaneous maintenance therapy in patients with CD, the efficacy of this therapy regarding disease location has not yet been investigated. “And we know that disease location may affect treatment outcomes of biologic therapies in CD,” explained Dr Peter Bossuyt (Imelda General Hospital, Belgium) [1,2]. Therefore, the current, post-hoc analysis used the data of the phase 3 ADVANCE (NCT03105128), MOTIVATE (NCT03104413), and FORTIFY (NCT03105102) trials to analyse the efficacy of risankizumab according to disease location [2].
Clinical remissiona at week 12 was higher in participants with colonic involvement (54.3%; n=190; P<0.001) and participants with ileal-colonic involvement (39.7%; n=252; P<0.001) who received risankizumab induction therapy compared with participants who received placebo (23.8% and 20.7%, respectively). In participants with ileal disease (n=85), a benefit of risankizumab was seen over placebo (33.7% vs 22.2%), although not significant. Similar results were reported for endoscopic responsesb and endoscopic remissionc at week 12.
Furthermore, risankizumab maintenance therapy significantly outperformed placebo in participants with colonic (54.0% [n=59] vs 37.1% [n=62]; P<0.05) or ileal-colonic involvement (53.3% [n= 67] vs 40.5% [n=79]; P<0.05), but not ileal disease (40% [n=15] vs 52.2% [n=23]), with regard to clinical remission at week 52. Dr Bossuyt added that endoscopic response, a more objective endpoint, did show benefits of risankizumab compared with placebo in participants with ileal disease (26.7% [n=15] vs 8.7% [n=23]). The number of participants with ileal disease in the maintenance analysis was low (n=38), thus these results should be interpreted with caution.
“This study confirms the efficacy of risankizumab in patients with moderately to severely active CD and confirms greater improvements in patients with colonic involvement,” said Dr Bossuyt. “Unfortunately, the treatment success is lower in participants with ileal disease, a pattern we have seen for other molecules as well. I believe that these results show us that we must recognise ileal and colonic Crohn’s disease as 2 separate conditions, extending beyond the difference in disease location.”
a. Clinical remission is defined as a Crohn's Disease Activity Index (CDAI) >150.
b. Endoscopic response is defined as a >50% decrease from baseline in SES-CD, or a 2-point reduction from baseline for patients with ileal disease and baseline SES-CD of 4.
c. Endoscopic remission was defined as a SES-CD ≤4 and at least a 2-point reduction vs baseline with no subscore greater than 1 in any individual variable.
- Rivière P, et al. Am J Gastroenterol. 2021;116(1):134–141.
- Bossuyt P, et al. Efficacy of risankizumab induction and maintenance therapy by baseline Crohn’s Disease location: Post hoc analysis of the phase 3 ADVANCE, MOTIVATE, and FORTIFY studies. OP40, ECCO 2022, 16–19 February.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Guselkumab plus golimumab promising combination for ulcerative colitis Next Article
Mirikizumab efficacious for active ulcerative colitis »
« Guselkumab plus golimumab promising combination for ulcerative colitis Next Article
Mirikizumab efficacious for active ulcerative colitis »
Table of Contents: ECCO 2022
Featured articles
Upadacitinib maintenance therapy delivers sustained improvements in active ulcerative colitis
Novel Treatment Modalities
Guselkumab shows encouraging safety and efficacy in ulcerative colitis
Guselkumab maintenance therapy achieved high efficacy rates in Crohn’s disease
Mirikizumab efficacious for active ulcerative colitis
Risankizumab more efficacious in colonic than in ileal Crohn’s disease
Guselkumab plus golimumab promising combination for ulcerative colitis
Combined endpoint may support personalised medicine in ulcerative colitis
Filgotinib seems promising for perianal fistulising Crohn’s disease
Upadacitinib maintenance therapy delivers sustained improvements in active ulcerative colitis
Upadacitinib counters extraintestinal manifestations in ulcerative colitis
Deucravacitinib does not meet primary endpoint for ulcerative colitis
Head-to-Head Comparisons
Anti-TNFs versus vedolizumab and ustekinumab in Crohn’s disease
Upadacitinib appears to be an efficacious therapy for moderately-to-severely ulcerative colitis
Subcutaneous infliximab versus subcutaneous vedolizumab in IBD
Vedolizumab outperforms anti-TNF in biologic-naïve ulcerative colitis
Short-Term and Long-Term Treatment Results
Ozanimod treatment shows maintained response in ulcerative colitis
Stopping infliximab but not antimetabolites leads to more relapses in Crohn’s disease
Vedolizumab first approved therapy for chronic pouchitis
VEDOKIDS: Vedolizumab seems effective in paediatric IBD
Primary endpoint of 5-hydroxytryptophan for fatigue in IBD not met
Specific Therapeutic Strategies
Positive outcomes with therapeutic drug monitoring during infliximab maintenance therapy
Segmental colectomy beneficial over total colectomy in Chrohn’s disease
Modified 2-stage ileal pouch-anal anastomosis versus 3-stage alternative
Similar results for different corticosteroid tapering protocols in UC
Miscellaneous Topics
Lessons from the COVID-19 pandemic for IBD management
AI model distinguishes between histologic activity and remission in ulcerative colitis
Multi-Omic and dietary analysis of Crohn’s disease identifies pathogenetic factors
Novel classification system for perianal fistulising Crohn’s disease
Vaccination tool associated with improved vaccination coverage in IBD
Comparable safety profiles of biological therapies in elderly patients with IBD
Early biologic therapy induces larger effect than delayed treatment in Crohn’s disease
RESTORE-UC: No better outcomes with FMT superdonors than with autologous stools
Related Articles
December 7, 2023
Obefazimod takes the spotlight as promising UC treatment
December 24, 2020
PPI therapy may render infliximab less effective in IBD patients
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

