"Many of the participants were on immune modifying therapies for IBD, but even after adjusting for the effects of these medications, the differences in antibody levels by vaccine type were still significant," coauthor Dr. Gil Y. Melmed of Cedars-Sinai Medical Center in Los Angeles told Reuters Health by email.
Among the 353 vaccine recipients with IBD and no prior COVID-19 infection, 148 (42%), 193 (55%), and 12 (3%) had been fully vaccinated with the Moderna, Pfizer, and Johnson & Johnson vaccines, respectively.
Demographic and disease characteristics were similar across vaccine groups (mean age 51 years, 62% female). Roughly 83% were taking biologics, Janus kinase-inhibitors, systemic corticosteroids, other immunomodulators, or some combination.
Antibody levels were measured at least two weeks and eight weeks after the final vaccine dose. At two weeks, positive antibody levels were detected in 121 (100%), 142 (99%), and 9 (90%) patients in the Moderna, Pfizer, and Johnson & Johnson groups, respectively.
At both two and eight weeks, however, antibody titers were significantly higher in the mRNA groups. At the later point, for example, quantitative log10 (anti-Spike IgG) levels were 3.72 in the Moderna group, 3.41 in the Pfizer group, and 2.65 in the Johnson & Johnson group.
On multivariate analysis, at weeks two and eight the vaccine type was independently associated with antibody levels, the researchers said. At week eight, lower titers were also independently associated both with a longer duration between completion of vaccine regimen and blood sampling, and with receipt of immunomodulatory therapy.
The finding of positive antibody levels "in virtually all IBD vaccine recipients," regardless of vaccine type and background treatment regimen, "is reassuring for patients with IBD, and supports existing literature that the vast majority of IBD patients, regardless of immunomodulatory therapy receipt, achieve positive humoral response to mRNA vaccines," the authors wrote.
"It is important to recognize that antibody responses after vaccination tell only one part of the story," Dr. Melmed added. "We did not measure T-cell responses which may be independent of antibody responses, and which represent an important component of the immune response to vaccines against the SARS-CoV-2 virus."
His team notes that their findings are limited by a small number of participants receiving the Johnson & Johnson shot and by a lack of racial and ethnic diversity in their cohort. Still, they conclude, their findings "are consistent with other immune compromised populations and have potential clinical ramifications" related to the need for booster vaccinations.
SOURCE: https://bit.ly/3g6SBg3 Gastroenterology, online August 12, 2021.
By Nancy Lapid
Posted on
Previous Article
« Acalabrutinib on par with ibrutinib, easier to tolerate in advanced CLL Next Article
Gastric cardia culprit in Barrett’s esophagus, transformative mechanism identified »
« Acalabrutinib on par with ibrutinib, easier to tolerate in advanced CLL Next Article
Gastric cardia culprit in Barrett’s esophagus, transformative mechanism identified »
Related Articles

October 23, 2019
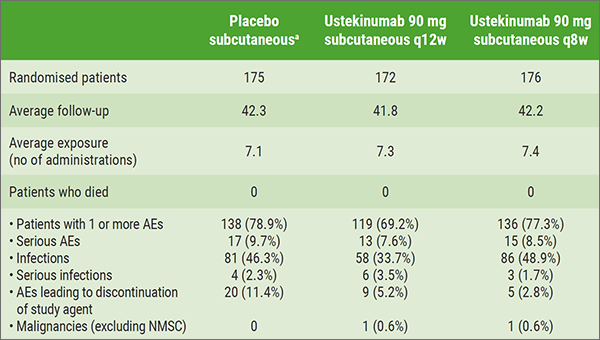
Subcutaneous ustekinumab as maintenance therapy in UC
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

