"The prevalence of IBS-type symptoms in IBD patients in remission is over three times higher than in the general population," Dr. Keeley M. Fairbrass of Leeds Gastroenterology Institute and the University of Leeds, in the U.K., told Reuters Health by email. "These patients exist in IBD clinics, and so we should be open-minded in our approach to managing patients with high symptomatology scores without evidence of disease activity."
Previous studies have suggested that IBD is a risk factor for developing IBS, but differentiating IBS-type symptoms from ongoing IBD activity can be difficult. A previous systematic review and meta-analysis of observational studies estimated the prevalence of IBS-type symptoms in IBD to be nearly 40% and indicated a higher prevalence in patients with Crohn's disease than in those with ulcerative colitis.
Dr. Fairbrass and colleagues updated the earlier systematic review but included only those studies that recruited patients with IBD who were deemed to be in remission.
Their review included 18 studies in addition to nine identified in the previous review. Overall, these 27 studies included 3,169 patients with IBD in remission.
The pooled prevalence of IBS-type symptoms among these patients with IBD in remission was 32.5% and was higher in patients with Crohn's disease (34.9%) than in patients with ulcerative colitis (28.9%), the researchers report in The Lancet Gastroenterology and Hepatology.
The prevalence of IBS-type symptoms was highest when a fecal calprotectin concentration of less than 100 ug/g was used to define remission (35.1%), but the prevalence was similar according to physician's global assessment (34.1%) and a validated disease-activity index (33.6%).
The prevalence was somewhat lower when remission was defined more strictly according to endoscopic (23.5%) or histologic assessment (25.8%).
The pooled prevalence of IBS-type symptoms differed according to symptom criteria: 31.5% in studies using Rome II criteria, 33.5% in those using Rome III criteria, and 29.6% in those using Rome IV criteria.
Anxiety scores, depression scores and somatic-symptom scores were significantly higher among patients who reported IBS-type symptoms than among those who did not.
"The reporting of symptoms in IBD may not be related to the presence of inflammatory disease activity, and escalating conventional pharmacotherapy in these patients is likely to be ineffective," Dr. Fairbrass said. "This study provides further evidence of the role of brain-gut interactions in patient with IBD and highlights that an integrated approach to the management of IBD patients, whereby targeting both inflammatory and psychological outcomes may be more appropriate."
"Improved characterization of this patient cohort is required before clinical trials of novel treatments can be considered," she said.
Dr. Hans Strid of Sahlgrenska Academy, University of Gothenburg, in Sweden, who wrote an editorial related to this report, told Reuters Health by email, "The most important finding in the updated meta-analysis and review, in my opinion, is that a stricter definition of remission results in lower prevalence of IBS-type symptoms in IBD. The prevalence is nevertheless high in comparison with the prevalence of IBS in the general population."
"A careful evaluation of GI symptoms in IBD patients by using biomarkers (fecal calprotectin and C-reactive protein), endoscopy, and occasionally radiology is mandatory," he said. "Psychological treatment, if available, can be used in IBD patients with IBS-type symptoms."
"The main message for physicians is to be aware of the high prevalence of IBS-type symptoms in patients with IBD and carry out a careful evaluation of GI symptoms," Dr. Strid said. "There is a need for randomized clinical trials of psychological and drug treatment of IBS-type symptoms in IBD."
By Will Boggs MD
SOURCE: https://bit.ly/2SD0RbI and https://bit.ly/3lnH8Jm The Lancet Gastroenterology and Hepatology, online October 1, 2020.
Posted on
Previous Article
« Asthma rescue with budesonide-formoterol cuts short-term flare risk Next Article
VA study finds more ALS hospitalizations with edaravone »
« Asthma rescue with budesonide-formoterol cuts short-term flare risk Next Article
VA study finds more ALS hospitalizations with edaravone »
Related Articles
January 26, 2021
COVID-19 vaccine recommended for all patients with IBD
April 14, 2020
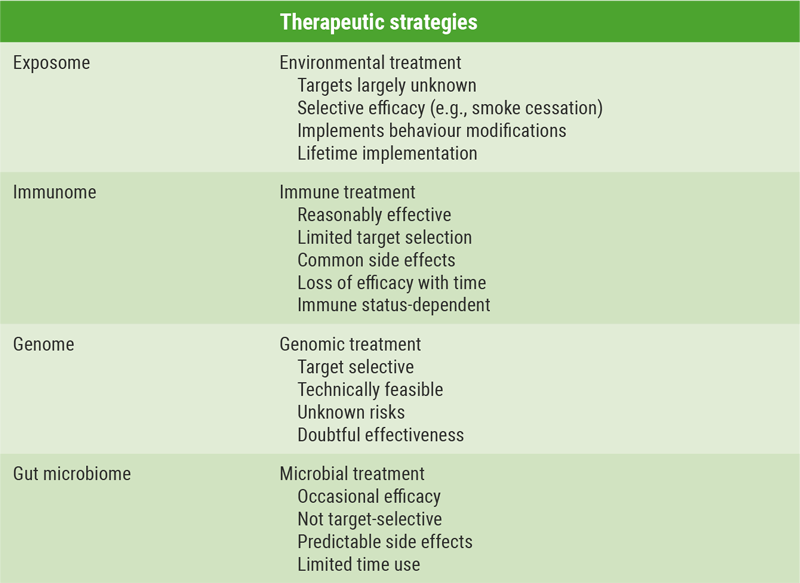
Possible new treatment targets in IBD
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

