Prof. Eric Simpson (Oregon Health & Science University, Portland, USA) covered systemic therapy in atopic dermatitis (AD) patients, an ever-evolving field [1]. But who needs it? In Prof. Simpson’s opinion, quality of life should be the determining factor. If it is still impaired when using topicals, AD patients should proceed to systemic treatment. “The choice of an agent should always depend on a shared decision-making with the patient,” Prof. Simpson recommended. Methotrexate remains a valuable choice for patients with moderate AD. “The IL-4/13 blocker dupilumab works well for the majority of our patients and is safe in the elderly,” he stated. Further options will be available in the near future, such as the selective IL-13 blocker tralokinumab, which has a more modest efficacy than dupilumab but good long-term efficacy.
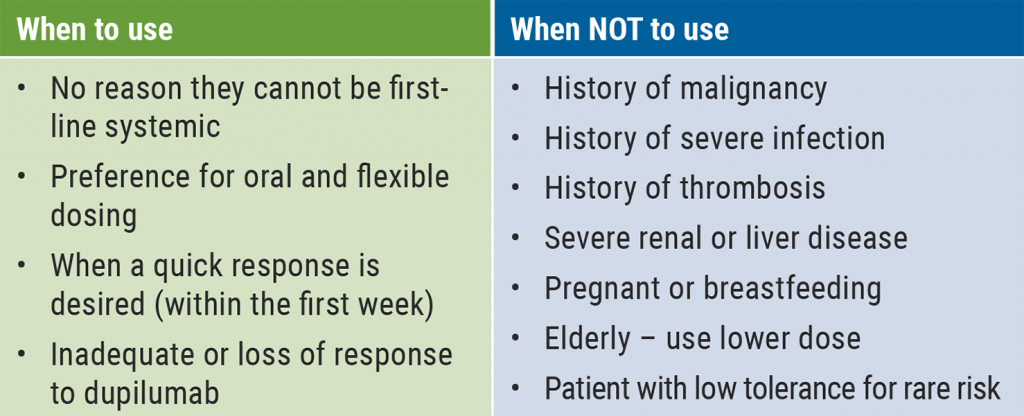
“Maybe we should not block 1 or 2 cytokines but multiple cytokines for the best effects,” Prof. Simpson said. This is the approach taken by JAK inhibitors. According to Prof. Simpson, these agents act more as immune modulators instead of having a single target like the biologics. “If a patient has a preference for oral dosing and a really quick response is warranted, that might be a good reason to use them,” he suggested. However, there are also various reasons to choose different agents (see Table). The JAK inhibitors baricitinib and upadacitinib have a black box warning for serious infections, malignancies, and thrombosis. Methotrexate has such a warning for liver disease. Thus, Prof. Simpson suggested using these agents cautiously. All JAK inhibitors improve itch rapidly, often within a day and faster than biologics, and all are appropriate as first-line therapy. Safety and tolerability issues to pay attention to are headache, acne, and herpes zoster. “My biggest concern with JAK inhibitors is venous thrombosis, this is what I look at most closely,” Prof. Simpson urged. The JAK-1/2 inhibitor baricitinib has the lowest efficacy of all JAK inhibitors but is well tolerated. “The efficacy of abrocitinib 100 mg is comparable with dupilumab; the higher dose is probably even better,” Prof. Simpson said.
Table: Systemic JAK inhibitors for AD [1]
Upadacitinib seems to have the highest efficacy of all JAK inhibitors. However, it has the least amount of published safety data. Acne is a unique side effect for upadacitinib observed in up to 17% of patients at a high dose. The risk of venous thrombosis is unknown. In a head-to-head study, 61% of patients treated with upadacitinib achieved an EASI 90 response at week 16 versus 39% with dupilumab. In addition, there was a 67% change from baseline in worst itch compared with 49% with dupilumab. “We have never seen this – but I need to see long-term safety data before I can state that this is the oral treatment of choice. Finally, there are great new options for your AD patients in 2021. Will they fill all the gaps? I sure hope so,” Prof. Simpson concluded.
- Simpson E. Systemic therapy in AD. Session S006: Atopic dermatitis. AAD VMX 2021, 23-25 April.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Nicotinamide and probiotics can support acne therapy Next Article
New therapeutic options add value to current acne treatment »
« Nicotinamide and probiotics can support acne therapy Next Article
New therapeutic options add value to current acne treatment »
Table of Contents: AAD 2021
Featured articles
Letter from the Editor
Late-Breaking Abstracts
Small molecule effective in moderate-to-severe psoriasis
Bruton’s tyrosine kinase inhibition promising for pemphigus vulgaris
Bimekizumab superior to secukinumab in psoriasis
Etrasimod – a new mode of action for treatment of atopic dermatitis
Women at higher risk for dermatologic side effects during immunotherapy
Novel easy-to-use foam formulation clears scalp psoriasis in one-third of patients
Anti-cholinergic gel demonstrates superior long-term tolerability and efficacy in axillary hyperhidrosis
Psoriasis – The Beat Goes On
Psoriasis: The treatment armamentarium continues to grow
Psoriasis management in times of COVID-19: the knowledge is growing steadily
Lower burden of high-risk atherosclerotic plaques in psoriasis patients treated with biologics
COVID-19: What Dermatologists Need to Know
Psoriasis and hidradenitis suppurativa during COVID-19: keep calm and carry on
COVID-19 in children – cutaneous involvement is common
Cutaneous reactions after COVID-19 vaccination: an update
Novel Developments in Sun Protection
Sunless tanning and other developments in sun protection
What Is Hot in Atopic Dermatitis
Comorbidity is common in adult and paediatric atopic dermatitis patients
Significant improvements in the system armamentarium for AD treatment
Topical pan-JAK inhibitor cream safe and efficacious in atopic dermatitis
Hairy Matters – What Is New in Alopecia
Allergies: an underrated factor in alopecia pathogenesis
Botulinum toxin A: a contradictory role in hair loss
Platelet-rich plasma in androgenetic alopecia – hype or hope?
Acne – New Developments
New therapeutic options add value to current acne treatment
Nicotinamide and probiotics can support acne therapy
Pearls of the Posters
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com


