“Diagnostic criteria for mask acne, often called ‘maskne’, were published recently,” explained Prof. Juliana Choi (Penn Dermatology Perlman, PA, USA) [1,2]. Mask acne is defined as the onset or exacerbation of acne over the area covered by a mask within 6 weeks of regularly wearing a face mask [2]. Differentials such as perioral dermatitis, seborrheic dermatitis, or rosacea must be excluded.
Limited data has been available on maskne, but a recent study including 30 acne and 36 rosacea patients demonstrated that COVID-19-related masks increased severity of both acne and rosacea. All participants wore masks on average 8 hours/day for 6 weeks [3]. “Masks flare both acne (in masked areas) and rosacea, but the causes are still not entirely clear,” Prof. Choi said. Based on observation, it appears a combination of acne mechanica due to the occlusion and friction of the face mask and tropical acne by heat and moisture. “The prolonged local pressure can cause poral occlusion. In addition, there is a rise of IL-1α due to the mechanical friction,” Prof. Choi explained. Each 1-degree rise in temperature results in a 10% increase in sebum production. A change in sebum composition can cause changes in the skin microbiome. Humidity leads to additional occlusion, irritation, and swelling of keratinocytes.
Two papers with recommendations for the management of maskne were published recently, both stating that maskne patients should clean their skin with a gentle antibacterial cleanser daily [4,5]. “Maintaining the skin barrier is important,” Prof. Choi said. Before and after wearing the mask, the skin should be moisturised – preferably several times a day. Moisturisers with ceramide or hyaluronic acid are particularly helpful. Those with oily or acne-prone skin should try a gel moisturiser. To prevent irritation, make-up under masks should be avoided – if this is not possible, non-comedogenic products are the best possible choice. Likewise, chemical sunscreens should not be applied under the mask. Whenever possible, 15 minutes mask breaks should be done every 4 hours. In these breaks, the skin can be moisturised. A new disposable mask should be used daily, cloth masks should be washed (without bleach) with a fragrance-free hypo-allergic laundry detergent. “Try to avoid irritating topicals such as retinoids. I have increased my use of non-antibiotic, anti-inflammatory agents, such as niacinamide, probiotics, and fish oil,” Prof. Choi suggested. Ivermectin cream is helpful for mask rosacea.
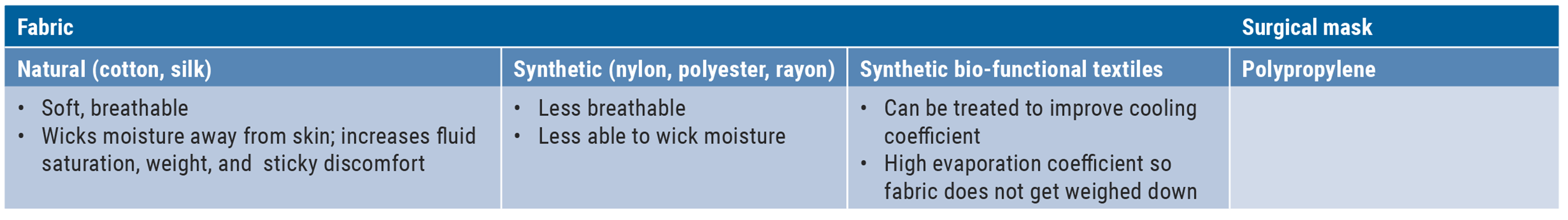
To avoid maskne, it is important that masks fit: they should be snug, but still comfortable. At present, there is no consensus about the best fabric, but natural materials and synthetic, bio-functional textiles are probably most convenient (see Table).
Table: Face mask material and skin interactions. Data from [4]
- Choi J. Diet, “Natural” Treatments, and Maskne. Session F002, AAD VMX 2021, 23-25 April.
- Teo WL. J Am Acad Dermatol 2021;84(2): 520-1.
- Damiani G, et al. Dermatol Ther 2021; Feb 19: e14848 [e-pub ahead of print].
- Teo WL. Int J Dermatol 2021;12 Feb; early view.
- Searle T, et al. Dermatol Ther 2021;34(1):e14589.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Meaningful amelioration of quality of life in paediatric AD patients on dupilumab Next Article
Platelet-rich plasma in androgenetic alopecia – hype or hope? »
« Meaningful amelioration of quality of life in paediatric AD patients on dupilumab Next Article
Platelet-rich plasma in androgenetic alopecia – hype or hope? »
Table of Contents: AAD 2021
Featured articles
Letter from the Editor
Late-Breaking Abstracts
Small molecule effective in moderate-to-severe psoriasis
Bruton’s tyrosine kinase inhibition promising for pemphigus vulgaris
Bimekizumab superior to secukinumab in psoriasis
Etrasimod – a new mode of action for treatment of atopic dermatitis
Women at higher risk for dermatologic side effects during immunotherapy
Novel easy-to-use foam formulation clears scalp psoriasis in one-third of patients
Anti-cholinergic gel demonstrates superior long-term tolerability and efficacy in axillary hyperhidrosis
Psoriasis – The Beat Goes On
Psoriasis: The treatment armamentarium continues to grow
Psoriasis management in times of COVID-19: the knowledge is growing steadily
Lower burden of high-risk atherosclerotic plaques in psoriasis patients treated with biologics
COVID-19: What Dermatologists Need to Know
Psoriasis and hidradenitis suppurativa during COVID-19: keep calm and carry on
COVID-19 in children – cutaneous involvement is common
Cutaneous reactions after COVID-19 vaccination: an update
Novel Developments in Sun Protection
Sunless tanning and other developments in sun protection
What Is Hot in Atopic Dermatitis
Comorbidity is common in adult and paediatric atopic dermatitis patients
Significant improvements in the system armamentarium for AD treatment
Topical pan-JAK inhibitor cream safe and efficacious in atopic dermatitis
Hairy Matters – What Is New in Alopecia
Allergies: an underrated factor in alopecia pathogenesis
Botulinum toxin A: a contradictory role in hair loss
Platelet-rich plasma in androgenetic alopecia – hype or hope?
Acne – New Developments
New therapeutic options add value to current acne treatment
Nicotinamide and probiotics can support acne therapy
Pearls of the Posters
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy