“Bruton’s tyrosine kinase (BTK) has a broad role in the rapid innate as well as the delayed adaptive immune response in pemphigus. Rilzabrutinib is not simply a BTK inhibitor, but it is a potent oral and reversible BTK inhibitor,” said Prof. Dedee F. Murrell (St George Hospital, University of New South Wales, Australia), explaining the rationale for the presented phase 2, proof-of-concept BELIEVE study (NCT02704429) [1-3]. The trial investigated rilzabrutinib for the treatment of newly diagnosed or relapsing pemphigus vulgaris [1].
The open-label study included 27 patients with a median age of 51. Among them, 33% were newly diagnosed and 67% relapsing. Concerning disease severity, 41% suffered from moderate pemphigus and 59% from moderate-to-severe pemphigus. The mean time from diagnosis was 8.9 years. Oral rilzabrutinib was administered at a dose of 400–600 mg twice daily while concomitant low-dose corticosteroids were allowed.
The primary endpoint was control of disease activity (CDA) after 4 weeks; secondary endpoints consisted of complete response rate, pemphigus disease area index (PDAI), decrease in steroid use, and quality of life. After 4 weeks, 52% of participants reached the primary CDA endpoint and this percentage increased to 70% after 12 weeks. After week 12, CDA was 67% in newly diagnosed and 72% in relapsing pemphigus patients. In moderate and moderate-to-severe grades at the same time point, CDA was 64% and 75%, respectively. “The CDA rates consistently improved over time, irrespective of pemphigus duration or the severity of pemphigus at onset,” Prof. Murrell elaborated.
Treatment with rilzabrutinib also improved PDAI scores significantly and reduced the extent of steroid use (see Figure). Overall, a clinically meaningful improvement in quality of life was found at week 12 compared with baseline, which stabilised during the post-treatment follow-up to week 24; the greatest effect was observed in the group of newly diagnosed patients.
Figure: Results for PDAI activity scores and use of corticosteroid in part A of the BELIEVE trial [1]
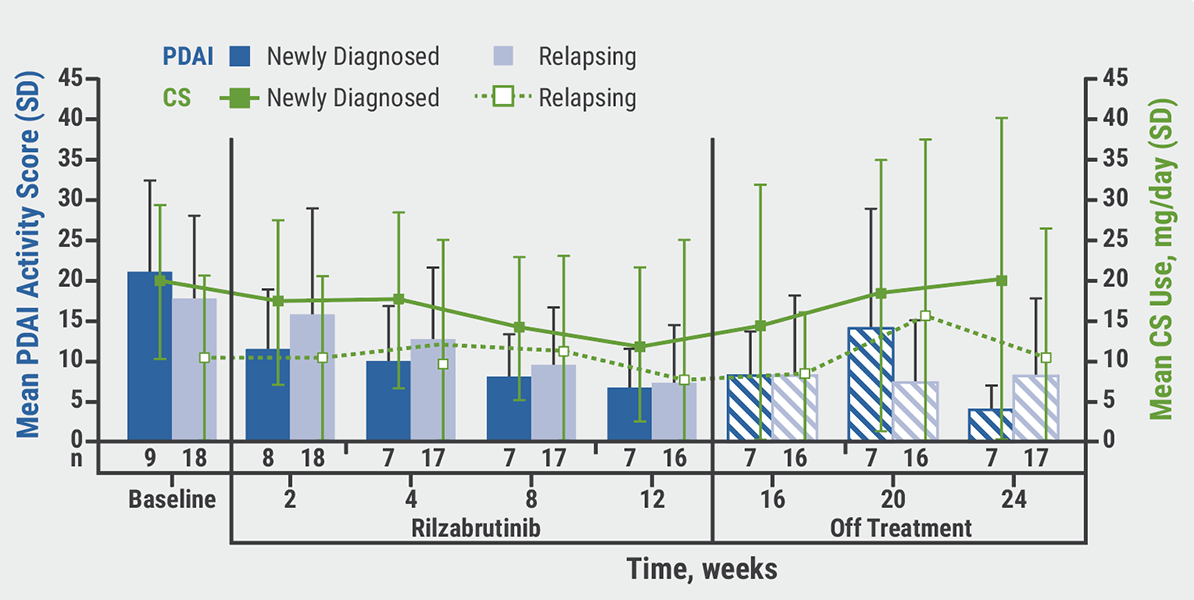
CS, corticosteroids; PDAI, pemphigus disease area index; SD, standard deviation.
“In terms of safety, we saw only transient and mild-to-moderate adverse events, giving an overall favourable risk-benefit profile,” said Prof. Murrell. Further results for rilzabrutinib will be seen in part B of BELIEVE and the ongoing phase 3 PEGASUS pivotal study (NCT03762265).
- Murrell D. Treatment with rilzabrutinib results in rapid and significant decrease in steroid use and improved quality of life in patients with chronic Relapsing Pemphigus: BELIEVE Phase II Study. Session S033, AAD VMX 2021, 23-25 April.
- Didona D, et al. Front Immunol. 2019;10:1418.
- Bradshaw JM, et al. Nat Chem Biol. 2015;11(7):525-31.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Bimekizumab superior to secukinumab in psoriasis Next Article
Small molecule effective in moderate-to-severe psoriasis »
« Bimekizumab superior to secukinumab in psoriasis Next Article
Small molecule effective in moderate-to-severe psoriasis »
Table of Contents: AAD 2021
Featured articles
Letter from the Editor
Late-Breaking Abstracts
Small molecule effective in moderate-to-severe psoriasis
Bruton’s tyrosine kinase inhibition promising for pemphigus vulgaris
Bimekizumab superior to secukinumab in psoriasis
Etrasimod – a new mode of action for treatment of atopic dermatitis
Women at higher risk for dermatologic side effects during immunotherapy
Novel easy-to-use foam formulation clears scalp psoriasis in one-third of patients
Anti-cholinergic gel demonstrates superior long-term tolerability and efficacy in axillary hyperhidrosis
Psoriasis – The Beat Goes On
Psoriasis: The treatment armamentarium continues to grow
Psoriasis management in times of COVID-19: the knowledge is growing steadily
Lower burden of high-risk atherosclerotic plaques in psoriasis patients treated with biologics
COVID-19: What Dermatologists Need to Know
Psoriasis and hidradenitis suppurativa during COVID-19: keep calm and carry on
COVID-19 in children – cutaneous involvement is common
Cutaneous reactions after COVID-19 vaccination: an update
Novel Developments in Sun Protection
Sunless tanning and other developments in sun protection
What Is Hot in Atopic Dermatitis
Comorbidity is common in adult and paediatric atopic dermatitis patients
Significant improvements in the system armamentarium for AD treatment
Topical pan-JAK inhibitor cream safe and efficacious in atopic dermatitis
Hairy Matters – What Is New in Alopecia
Allergies: an underrated factor in alopecia pathogenesis
Botulinum toxin A: a contradictory role in hair loss
Platelet-rich plasma in androgenetic alopecia – hype or hope?
Acne – New Developments
New therapeutic options add value to current acne treatment
Nicotinamide and probiotics can support acne therapy
Pearls of the Posters
Related Articles

September 4, 2019
Etanercept and methotrexate as first-line treatment in PsA
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

