https://doi.org/10.55788/948cc8a4
“Severe side effects with JAK inhibitor therapy are probably less common in atopic dermatitis (AD) patients than in the elderly rheumatoid population, but the risk is not zero. We see herpes infections as a class-wide phenomenon,” said Prof. Jonathan Silverberg (George Washington University School of Medicine, Washington DC, USA) in his talk on JAK inhibitors in AD [1]. However, the rates of herpes zoster infections were relatively low in AD trials with abrocitinib, baricitinib, and upadacitinib. Though it should be noted that patients with disseminated herpes zoster and herpes simplex infections and those with recurrent, localised herpes zoster and a history of eczema herpeticum were excluded from the studies. “If you treat these patients, the rates of herpes zoster are expected to be higher,” Prof. Silverberg warned. Therefore, if indicated, patients should receive a herpes zoster vaccine before treatment with a JAK inhibitor.
In Prof. Silverberg’s opinion, age is a big risk factor for therapy with all JAK inhibitors. Side effects differ between the different JAK inhibitors, even between selective JAK1 inhibitors. In patients treated with upadacitinib, in a real-world scenario, there is a stronger acne signal: about 10% of patients will get acne. “But patients are finally itch-free, so they do not care about acne. It is a mixed bag, sometimes patients develop folliculitis on the back,” Prof. Silverberg said. Patients treated with abrocitinib also often suffer from nausea. Overall, the safety profile of these 2 agents is fairly comparable.
Always start with the lower dose
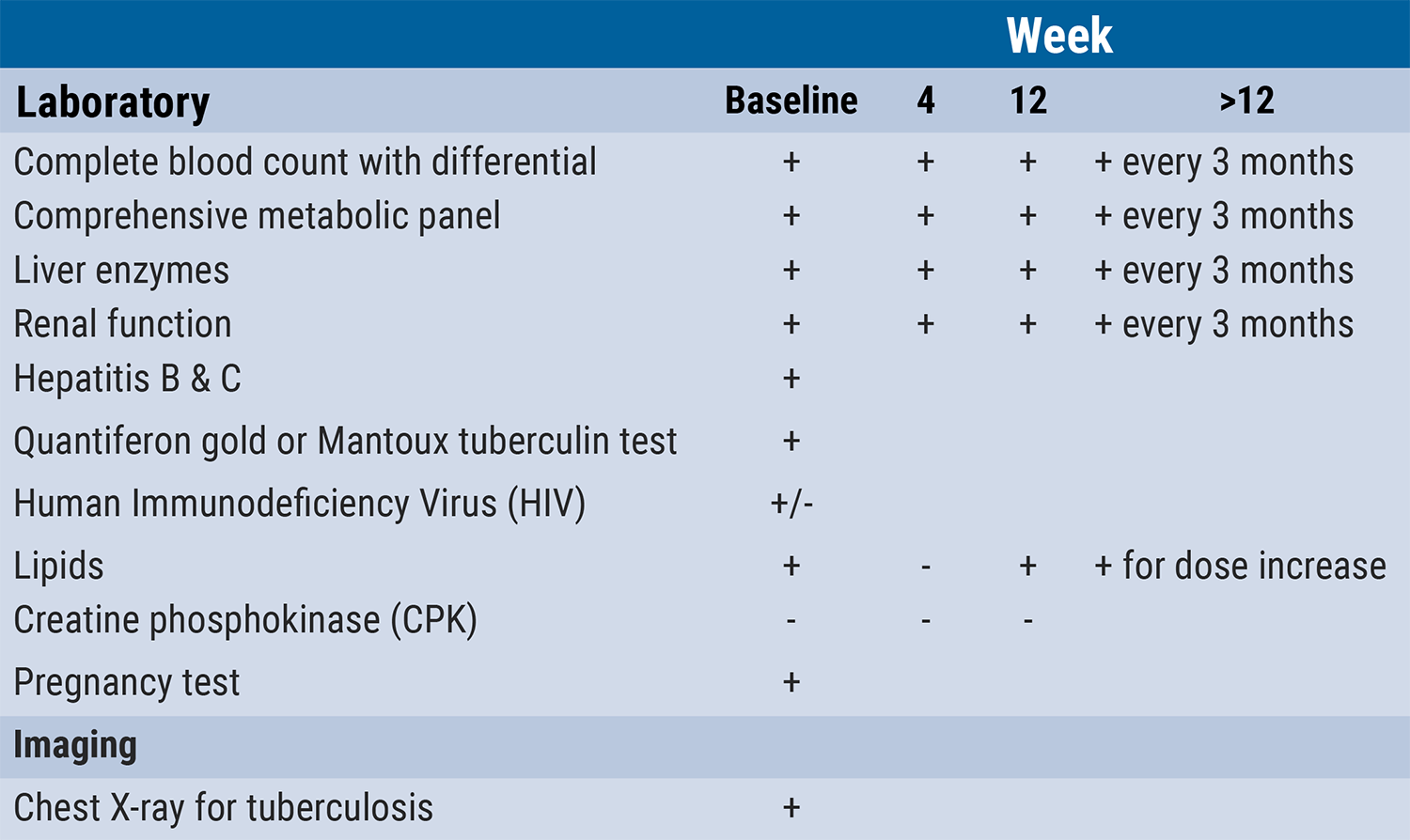
Prof. Silverberg recommended starting with the lower dose (i.e. abrocitinib 100 mg, upadacitinib 15 mg), and to increase in case of an inadequate response. In general, only low doses should be used in both adolescents and seniors. Recently, 29 rheumatologists developed a set of lab checks in a consensus statement (see Table). “The recommendation is to monitor patients, even if it is unnecessary 95% of the time,” Prof. Silverberg concluded.
Table: What and when to check during JAK inhibitor therapy. Derived from [2]
- Silverberg JI. Atopic Dermatitis. F074, AAD 2022 Annual Meeting, 25–29 March, Boston, MA, USA.
- Nash P, et al. Ann Rheum Dis 2021;80:71–87.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Intestinal microbe-preparation: Modest activity but safe for mild psoriasis Next Article
JAK inhibitors: A risk assessment »
« Intestinal microbe-preparation: Modest activity but safe for mild psoriasis Next Article
JAK inhibitors: A risk assessment »
Table of Contents: AAD 2022
Featured articles
Letter from the Editor
Lebrikizumab treatment leads to encouraging outcomes in multiple traits of AD
New Developments and Unmet Needs in Dermatology
Light at the end of the tunnel for vitiligo therapy
Intestinal microbe-preparation: Modest activity but safe for mild psoriasis
Alopecia areata: 1-year baricitinib treatment increases success
New anticholinergic preparation is effective and tolerable in hyperhidrosis
What’s Hot in Rare Diseases
Add-on apremilast may improve recalcitrant dermatomyositis
Could dupilumab put an end to the therapeutic draught in prurigo nodularis?
Fungal skin infections in children: A diagnosis to keep in mind
Innovative gel speeds up clearance of molluscum contagiosum lesions
JAK inhibition offers promising treatment prospects for uncommon dermatoses
JAK inhibitors may offer a new horizon in the treatment of sarcoidosis
Psoriasis: State of the Art
New insights into psoriasis comorbidity
Long-term psoriasis treatment with bimekizumab results in maintained efficacy
Novel developments in topical psoriasis therapy
Atopic Dermatitis: Novel Agents Enter the Stage
JAK inhibitors in AD: Setting the efficacy bar even higher
Lebrikizumab treatment leads to encouraging outcomes in multiple traits of AD
Novel IL-4/IL-13 blocker shows high efficacy with only modest conjunctivitis signal
Posters
Inpatient dermatologic therapy is linked to lower mortality and readmission rates
AD treatment during the pandemic: dupilumab does not raise COVID-19 infection risk
Upadacitinib: Fast and more pronounced skin improvement in AD patients
Dermatology diseases need the highest doses of biologics
Related Articles
May 9, 2019
IBD risk of treatment with IL-17 antagonists
April 22, 2024
GUIDE demonstrates: Hit hard and early in psoriasis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

