Published in the Journal of the American College of Cardiology, the consensus decision pathway focuses on myocarditis and other types of myocardial involvement, patient-centered approaches for long COVID and guidance on resuming exercise following COVID-19.
"The best means to diagnose and treat myocarditis and long COVID following SARS-CoV-2 infection continues to evolve," Dr. Ty Gluckman, co-chair of the expert consensus decision pathway, says in a news release.
"This document attempts to provide key recommendations for how to evaluate and manage adults with these conditions, including guidance for safe return to play for both competitive and non-competitive athletes," he adds.
Myocarditis is now recognized as a rare but serious complication of SARS-CoV-2 infection as well as COVID-19 mRNA vaccination.
"Because myocarditis is associated with a heightened risk of cardiac complications early in the disease course, a proactive management plan should be in place," the panel says.
They recommend that patients with mild or moderate myocarditis be hospitalized to closely monitor for worsening symptoms, while undergoing tests and treatment.
They advise that patients with severe myocarditis ideally be hospitalized at centers with expertise in advanced heart failure, mechanical circulatory support and other advanced therapies.
Long COVID
The panel also addresses post-acute sequelae of SARS-CoV-2 infection (PASC), which has been reported in up to 30% of people infected with the novel coronavirus.
Symptoms of so-called "long COVID" can be wide-ranging and include fatigue, "brain fog", sleep disorders, fevers, gastrointestinal symptoms, anxiety, and depression. Symptoms can persist for months and can range from mild to incapacitating.
The ACC consensus document focuses on the cardiac sequelae of long COVID, which may include tachycardia, exercise intolerance, chest pain and shortness of breath.
They propose the following two terms to better understand potential etiologies for those with cardiovascular symptoms of long COVID:
- PASC-CVD, or PASC-Cardiovascular Disease, refers to a broad group of cardiovascular conditions (including myocarditis) that develop at least four weeks after COVID-19 infection.
- PASC-CVS, or PASC-Cardiovascular Syndrome, includes a wide range of cardiovascular symptoms without objective evidence of cardiovascular disease following standard diagnostic testing.
In general, patients with long COVID and cardiovascular symptoms should undergo evaluation with laboratory tests, electrocardiogram (ECG), echocardiogram, ambulatory rhythm monitor and/or additional pulmonary testing based their symptoms, the panel says.
They recommend consultation with a cardiologist when test results are abnormal, with additional evaluation based on the suspected clinical condition, such as myocarditis.
Because multiple factors likely underlie PASC-CVS, evaluation and management should be driven by the predominant cardiovascular symptom(s), the panel says.
For patients with tachycardia and exercise intolerance, increased bed rest and/or a decline in physical activity may trigger cardiovascular deconditioning with progressive worsening of symptoms, they advise.
"There appears to be a 'downward spiral' for long COVID patients. Fatigue and decreased exercise capacity lead to diminished activity and bedrest, in turn leading to worsening symptoms and decreased quality of life," panel co-chair Dr. Nicole Bhave adds in the news release.
"The writing committee recommends a basic cardiopulmonary evaluation performed upfront to determine if further specialty care and formalized medical therapy is needed for these patients," Dr. Bhave says.
For patients with PASC-CVS and tachycardia and exercise intolerance, upright exercise (walking or jogging) should be replaced with recumbent or semi-recumbent exercise (rowing, swimming or cycling) to avoid worsening fatigue.
Exercise intensity and duration should be low at first and gradually increase over time, with a transition back to upright exercise as symptoms improve.
Additional interventions such as increased salt and fluid intake, elevation of the head during sleep and support stockings, or/and drug therapy such as beta-blockers, should be considered on an individual basis, the panel advises.
Return To Play
The panel also addresses the issue of when it might be safe for athletes (and exercise enthusiasts) to get back in the game after a hospital stay for COVID-19.
For athletes recovering from COVID-19 with ongoing cardiopulmonary symptoms (chest pain, shortness of breath, palpitations, lightheadedness) or those requiring hospitalization with increased suspicion for cardiac involvement, the panel advises further evaluation with an ECG, cardiac troponin measurement and an echocardiogram.
For those with abnormal test results, further evaluation with cardiac magnetic resonance imaging should be considered; athletes found to have myocarditis should abstain from exercise for three to six months, the panel says.
They advise against cardiac testing for asymptomatic individuals following COVID-19 infection. Individuals should abstain from training for three days to ensure that symptoms do not develop.
For those with mild or moderate non-cardiopulmonary symptoms (fever, lethargy, muscle aches), exercise training can resume after symptoms resolve.
For those who are at least three months beyond their COVID infection without ongoing cardiopulmonary symptoms, a gradual increase in exercise is recommended without the need for cardiac testing.
Based on the low prevalence of myocarditis found in competitive athletes with COVID-19, the panel says these recommendations can be reasonably applied to high-school athletes and adult recreational exercise enthusiasts.
They call for further studies to better understand how long cardiac abnormalities persist following COVID-19 infection and the role of exercise training in long COVID.
SOURCE: https://bit.ly/3CNlfNr Journal of the American College of Cardiology, online March 16, 2022.
By Reuters Staff
Posted on
Previous Article
« Serious mental illness tied to increased CV risk, starting in young adulthood Next Article
Experimental lupus therapy only shows significant effect at highest dose »
« Serious mental illness tied to increased CV risk, starting in young adulthood Next Article
Experimental lupus therapy only shows significant effect at highest dose »
Related Articles
January 18, 2021
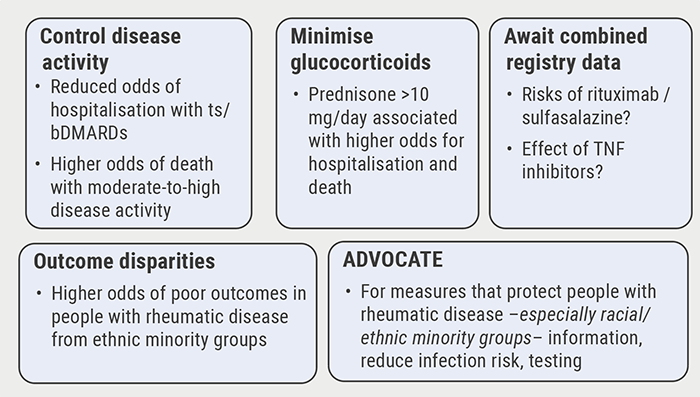
Poor disease control: a risk factor for severe COVID-19
December 6, 2021
Cancer patients benefit from mRNA vaccines
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

