https://doi.org/10.55788/42123d44
The current ESC Guidelines recommend DAPT with aspirin plus a potent P2Y12 inhibitor over 12 months after ACS and PCI [1]. The current ULTIMATE-DAPT trial (NCT03971500) investigated the consequences of reducing DAPT to ticagrelor monotherapy after 1 event-free month post-PCI on DAPT [2,3]. The 2 primary endpoints, evaluated through 1 year, were non-inferiority in MACCE (i.e. cardiac death, myocardial infarction, ischaemic stroke, definite stent thrombosis, clinically driven target vessel revascularisation) and superiority in bleedings of types 2, 3, or 5 according to the Bleeding Academic Research Consortium (BARC).
The multinational trial randomised 3,400 adults after 30 days with aspirin plus ticagrelor to either continue this regimen or switch to the P2Y12 inhibitor plus placebo over 1 year. The trial cohort had a median age of around 63 years and slightly over 25% were women. “70% of the patients had single vessel disease and about 1.3 lesions were treated per patient,” added Prof. Gregg Stone (Icahn School of Medicine at Mount Sinai, NY, USA).
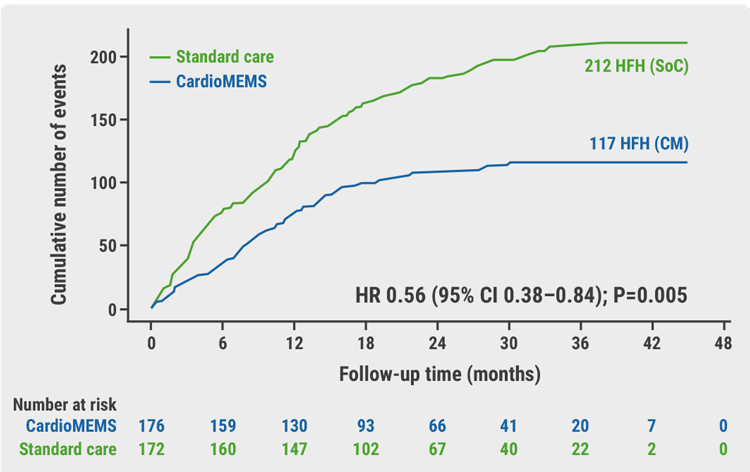
The primary endpoint of type 2, 3, or 5 BARC bleedings occurred in 2.1% on ticagrelor only and 4.6% on continued DAPT (HR 0.45; 95% CI 0.30–0.66; P<0.0001; see Figure). The rates of MACCE in both treatment groups were low and were not significantly different: on ticagrelor plus aspirin, 3.7% of the participants experienced a MACCE compared with 3.6% in the ticagrelor plus placebo group (HR 0.98; 95% CI 0.69–1.39; Pnon-inferiority<0.0001). Of note, the upper confidence interval was 1.39 reflecting a relatively low number of events. The P-value was for non-inferiority with a prespecified margin of 5. Statistical significance was not established for all secondary MACCE endpoints.
Figure: Primary endpoint of BARC types 2, 3, or 5 bleeding in the ULTIMATE-DAPT study [2]
 Blee
BleeBARC, Bleeding Academic Research Consortium; CI, confidence interval; HR, hazard ratio.
“These results, in concert with prior trials, warrant an update to the guidelines and a change in practice to treat most patients with ACS after PCI with 1 month only on DAPT, followed by conversion to single antiplatelet therapy with a potent P2Y12 inhibitor, with the strongest evidence to date supporting ticagrelor,” Prof. Stone concluded. While de-escalating aspirin has been shown clearly to reduce bleeding, very large trials would be needed to exclude harm in terms of increased ischaemic risk as evidenced by the wide confidence intervals observed in the trial.
- Byrne RA, et al. Eur Heart J 2023;44(38):3720-3826.
- Ge Z, et al. Lancet 2024;403(10439):1866–1878.
- Stone GW, et al. One-month ticagrelor monotherapy after PCI in acute coronary syndromes: principal results from the double-blind, placebo-controlled ULTIMATE-DAPT trial. LB3, Session 406, ACC 2024 Scientific Session, 6–8 April, Atlanta, USA.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« AEGIS-II: ApoA-1 did not reduce MACE in patients with myocardial infarction but may provide benefit in patients with high LDL levels Next Article
Addressing frailty in patients undergoing TAVR »
« AEGIS-II: ApoA-1 did not reduce MACE in patients with myocardial infarction but may provide benefit in patients with high LDL levels Next Article
Addressing frailty in patients undergoing TAVR »
Table of Contents: ACC 2024
Featured articles
Matters of the heart: late-breaking news from the American College of Cardiology
Heart Failure and Cardiomyopathy
STEP-HFpEF DM: Semaglutide beneficial in patients with HFpEF and diabetes
IMPROVE-HCM: Promising results for ninerafaxstat in non-obstructive HCM
Acute Coronary Syndrome and Acute Myocardial Infarction
ACS: Necessary DAPT after PCI may be shorter than currently advised
AEGIS-II: ApoA-1 did not reduce MACE in patients with myocardial infarction but may provide benefit in patients with high LDL levels
REDUCE-AMI: Re-evaluating the role of routine beta-blockade in patients with acute myocardial infarction
Interventional Cardiology in 2024
Self-expanding versus balloon-expendable TAVR in patients with small aortic annuli
Safety of TAVI non-inferior to SAVR for patients with lower surgical risk
Interatrial shunt for HF: neutral primary endpoint but potential benefit in HFrEF
Peripheral artery disease: procedure-guidance by IVUS superior to angiography
IVUS-guided PCI beats angiography in patients with acute coronary syndrome
Addressing frailty in patients undergoing TAVR
Novel Developments in Risk Factor Management
Preventive PCI of vulnerable intracoronary plaque leads to favourable outcomes
KARDIA-2: Add-on zilebesiran effectively lowers blood pressure
BRIDGE-TIMI 73a: Olezarsen halves triglyceride levels
Plozasiran: A novel approach to severe hypertriglyceridaemia
High-risk and very high-risk patients meet LDL-cholesterol targets with lerodalcibep
No cardioprotective effect of ACE inhibitors in patients with cancer
Best of Posters
SGLT2 inhibition in heart failure more advantageous for women than men
Anxiety and depression: Lifestyle influential in MACE prevention
Meet the Trialists
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com