The authors of the study in the New England Journal of Medicine also report that they have brought down the cost of unspooling the complete genetic code of a tumor to a level that's comparable to the costs of conventional testing.
In addition, the technique may be useful in treating solid tumors.
"We showed that whole-genome sequencing has advanced to the point where, if you apply it in a way that we have, it's useful, accurate, practical and accessible for routine testing," Dr. David Spencer of Washington University School of Medicine in St. Louis, Missouri, told Reuters Health by phone. "We can, in a matter of days, sequence the entire genome and distill it down to a one-page report that provides leukemia doctors with what they need to know to move forward with treatment."
The study looked at bone marrow aspirate or peripheral blood from 117 newly diagnosed patients and analyzed stored samples from 146 others. Because it was a proof-of-concept study, none of the results were passed back to the patients or their doctors.
The whole-genome findings were significant enough to have changed the risk category for 16% of the 117 newly diagnosed patients. In most cases, the researchers say, the results would have resulted in more-aggressive treatment.
When they focused on 68 consecutive patients with acute myeloid leukemia (AML), whole-genome testing produced new findings in 25% of the cases and redefined the risk category in 15% of patients.
Whole-genome results were generally available in five days - sometimes in three days - at a cost of about $1,900, compared to $1,000 to $2,000 for conventional genetic testing in a typical AML patient. Conventional genetic testing usually required 10 days, said Dr. Spencer, an assistant professor of medicine and also medical director of the clinical sequencing facility at the McDonnell Genome Institute.
"The next step is to use this in the context of a clinical study," which is in the planning stages, he said. "We think this approach is valuable and will help oncologists and patients."
Over the longer term, "Whole-genome sequencing can be performed on DNA from tissue biopsy samples of solid tumors, which are often insufficient for standard molecular assays and difficult to culture for cytogenetic studies," the researchers write. "The benefits could be even greater for these cancer types, in which whole-genome sequencing could be used to rapidly survey the entire genome for an expanding number of key mutations and structural alterations with only a small amount of DNA."
"Such an approach would simplify genomic testing for these patients and probably increase the yield of clinically relevant findings, which may ultimately improve the precision of approaches for treating many patients with cancer," they write.
SOURCE: https://bit.ly/3sZAU69 The New England Journal of Medicine, online March 10, 2021.
By Gene Emery
Posted on
Previous Article
« Bone mineral density screening may benefit kidney stone patients Next Article
Pediatric atopic dermatitis tied to school, work absenteeism »
« Bone mineral density screening may benefit kidney stone patients Next Article
Pediatric atopic dermatitis tied to school, work absenteeism »
Related Articles

February 18, 2021
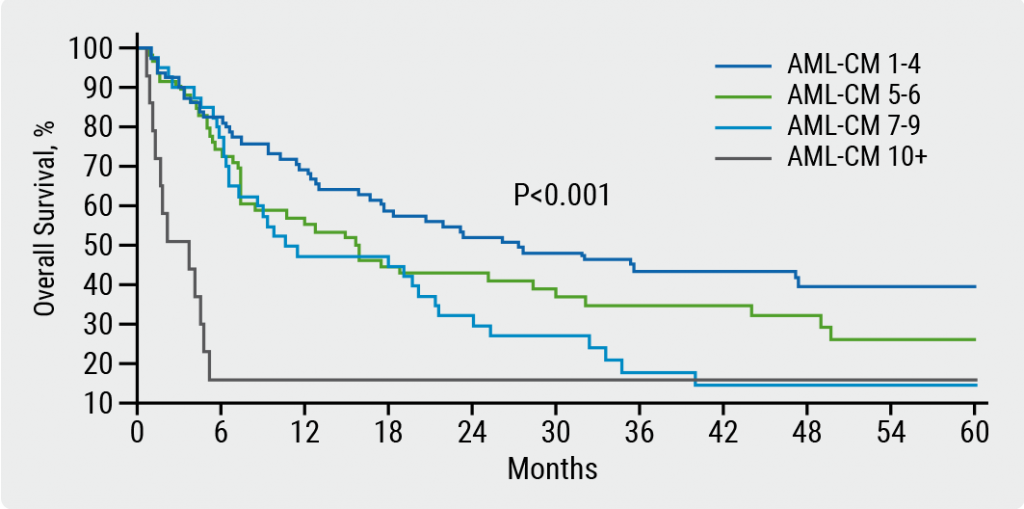
Prognostic validity of AML composite model in predicting mortality
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

