The guidelines were published online simultaneously in the European Heart Journal together with a companion question-and-answer document [2,3]. The guidelines are aimed at the treatment and diagnosis for “patients with acute chest discomfort but no persistent ST-segment elevation ACS, who exhibit ECG changes that may include transient ST-segment elevation, persistent or transient ST-segment depression, T-wave inversion, flat T waves, or pseudo-normalisation of T waves; or their ECG may be normal” [2].
Firstly, the new streamlined workflow for diagnosis of suspected NSTE-ACS includes the use of high-sensitivity troponin. Prof. Collet remarked, “In these guidelines, we have implemented the use of high-sensitivity troponins everywhere with the 0/1-hour algorithm, when available.” Recent evidence summarised in the guidelines supports the value of high-sensitivity troponin to signal MI within 2 hours.
Secondly, non-invasive imaging in low-risk patients should be the preferred approach. “If you rule out the diagnosis of MI but there is still a suspicion of underlying disease, you may use CT angiography. It’s very helpful,” Prof. Collet said. It avoids invasive angiography in around 30% of cases, and has moved up to a class I, level A recommendation to exclude ACS when there is a low-to-intermediate likelihood of coronary artery disease and troponin tests or ECG results are normal or inconclusive.
Thirdly, risk stratification has been overhauled to simplify timely triage and intervention. The previous 4 risk groups have been simplified to 3. Patients who require a trip to the cath lab within 2 hours fall into the very-high risk group. High-risk patients require invasive management within 24 hours—during this time CT angiography may be performed. Low-risk patients are those for whom invasive management is selective.
The fourth take-home message presented by Prof. Collett is the timing of antithrombotic treatment, possibly the most controversial of the changes. The advice is to “avoid pre-treatment” when invasive management will be performed anyway, Prof. Collet stressed. “This is an important recommendation. We do not want to use potent P2Y12 inhibitors when the diagnosis of NSTEMI is not established in terms of coronary anatomy.” The evidence from several trials were pooled to support this recommendation.
Lastly, entirely new guidelines have been prepared for special populations, including MINOCA, spontaneous coronary artery dissection, and quality indicators in NSTE-ACS care, including diagnosis, care pathway, and medical intervention.
To summarise, new key recommendations for NSTE-ACS are listed below [2]. The major changes in recommendations from 2015 to 2020 are summarised in the Table.
Diagnosis
- As an alternative to the ESC 0/1-hour algorithm, it is recommended to use the ESC 0/2-hour algorithm with blood sampling at 0 and 2 hours, if a high-sensitivity cardiac troponin (hs-cTn) test with a validated 0/2-hour algorithm is available.
- It is not recommended to routinely measure additional biomarkers, such as CK, CK-MB, h-FABP, or copeptin, in addition to hs-cTn for diagnostic purposes.
- To gain prognostic information, measuring BNP or NT-proBNP plasma concentrations should be considered.
- Prasugrel should be considered for NSTE-ACS patients who proceed to PCI.
- Routine pre-treatment with a P2Y12 receptor inhibitor is not recommended for patients in whom the coronary anatomy is not known and for whom early invasive management is planned.
- In patients with NSTE-ACS who cannot undergo an early invasive strategy, pre-treatment with a P2Y12 receptor inhibitor may be considered depending on bleeding risk.
- De-escalation of P2Y12 inhibitor treatment (e.g. with a switch from prasugrel or ticagrelor to clopidogrel) may be considered as an alternative DAPT strategy, especially for ACS patients deemed unsuitable for potent platelet inhibition. De-escalation may be done unguided based on clinical judgement or guided by platelet function testing or CYP2C19 genotyping depending on the patient’s risk profile and availability of respective assays.
- In patients with AF (CHA2DS2-VASc score ≥1 in men and ≥2 in women), after a short period of triple antithrombotic therapy (up to 1 week from the acute event), DAT is recommended as the default strategy using a DOAC at the recommended dose for stroke prevention and single oral antiplatelet agent (preferably clopidogrel).
- Discontinuation of antiplatelet treatment in patients treated with OACs is recommended after 12 months.
- DAT with an OAC and either ticagrelor or prasugrel may be considered as an alternative to triple antithrombotic therapy with an OAC, aspirin, and clopidogrel in patients with a moderate or high risk of stent thrombosis, irrespective of the type of stent used.
- An early invasive strategy within 24 hours is recommended in patients with any of the following high-risk criteria:
- diagnosis of NSTEMI;
- dynamic or presumably new contiguous ST/T-segment changes suggesting ongoing ischaemia;
- transient ST-segment elevation; or
- a GRACE risk score of >140.
- A selective invasive strategy after appropriate ischaemia testing or detection of obstructive CAD by coronary CT angiography is recommended in low-risk patients.
- Delayed, as opposed to immediate, angiography should be considered in haemodynamically stable patients without ST-segment elevation successfully resuscitated after an out-of-hospital cardiac arrest.
- Complete revascularisation should be considered in NSTE-ACS patients without cardiogenic shock and with multivessel CAD.
- Complete revascularisation during index PCI may be considered in NSTE-ACS patients with multivessel disease.
- Fractional flow reserve-guided revascularisation of non-culprit NSTE-ACS lesions may be used during index PCI.
Table: Key changes from 2015 to 2020 in NSTE-ACS recommendations. Modified from [2]
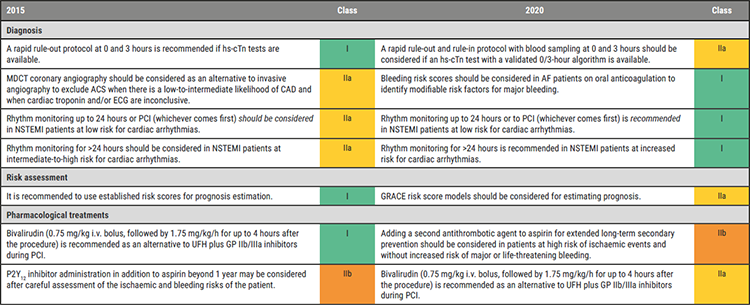
Collet JP, et al. 2020 ESC Guidelines on non-ST-segment evaluation acute coronary syndromes. 2020 New ESC Guidelines, ESC Congress 2020, 30 Aug.ACS, acute coronary syndromes; BNP, B-type natriuretic peptide; CAD, coronary artery disease; CCTA, coronary computed tomography angiography; ECG, electrocardiogram/electrocardiography; GP, glycoprotein; GRACE, Global Registry of Acute Coronary Events; hs-cTn, high-sensitivity cardiac troponin; i.v., intravenous; MDCT, multidetector computed tomography; NSTEMI, non-ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; UFH, unfractionated heparin.
Posted on
Previous Article
« 2020 Sports Cardiology and Exercise in Cardiovascular Patients Guidelines Next Article
2020 Atrial Fibrillation Guidelines »
« 2020 Sports Cardiology and Exercise in Cardiovascular Patients Guidelines Next Article
2020 Atrial Fibrillation Guidelines »
Table of Contents: ESC 2020
Featured articles
2020 ESC Clinical Practice Guidelines
2020 Atrial Fibrillation Guidelines
2020 Non-ST-Segment Elevation Acute Coronary Syndromes Guidelines
2020 Sports Cardiology and Exercise in Cardiovascular Patients Guidelines
2020 Adult Congenital Heart Disease Guidelines
Hot Line Presentations
SGLT2 inhibitor improves cardiovascular outcomes in heart failure patients
First-in-class cardiac myosin inhibitor effective in obstructive hypertrophic cardiomyopathy
Reduced cardiovascular outcomes with early rhythm control
Trimetazidine after successful PCI not associated with fewer cardiac events
POPular TAVI: Aspirin-only antiplatelet strategy?
Reduced NT-proBNP in HFpEF with sacubitril/valsartan
DAPA-CKD: Dapagliflozin improves CKD survival ± diabetes
Low-dose colchicine reduces CV death and ischaemic events in coronary disease
Similar outcomes sPESI and HESTIA for pulmonary embolism triage
Antihypertensives also reduce CV risk in people with normal blood pressure
COVID-19: Continuing versus suspending ACE inhibitors and ARBs
Drug initiation strategy not associated with increased use of oral anticoagulants
Restrictive blood transfusion non-inferior and cost-effective strategy
Late-Breaking Science
Increased mortality with colchicine in patients with ACS
Rivaroxaban protects limbs and ischaemic events in CAD-PAD patients
Antisense APOC3 oligonucleotide lowers triglyceride and atherogenic lipoproteins
Antisense ANGPTL3 lowers triglycerides
Reduced progression of coronary atherosclerosis with icosapent ethyl
Digoxin improves symptoms in stable patients with permanent AF
SGLT2 inhibitor ertugliflozin shows similar mortality but fewer HF hospitalisations
COVID and Cardiovascular Disease
Risk factors for thromboembolism and bleeding in COVID-19: lessons from Wuhan
The Yale COVID-19 Cardiovascular Registry
COVID-19 treatments and the importance of randomised trials
Related Articles
November 5, 2020
2020 Adult Congenital Heart Disease Guidelines
November 5, 2020
2020 Non-ST-Segment Elevation Acute Coronary Syndromes Guidelines

November 5, 2020
Reduced NT-proBNP in HFpEF with sacubitril/valsartan
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

