https://doi.org/10.55788/2ec9a13b
Breast cancer treatment is associated with cancer-related cognitive impairment. However, the effect of endocrine therapy versus chemotherapy followed by endocrine therapy (chemo-endocrine therapy) is not well understood, nor is the impact of menopausal status [1,2]. Therefore, the impact of breast cancer treatment on cognition was explored in the RxPONDER PRO substudy (NCT01272037).
In this substudy, the 8-item Patient-Reported Outcomes Measurement Information System (PROMIS) Perceived Cognitive Function Concerns (PCF) questionnaire was completed at baseline and after 6, 12, and 36 months after randomisation of 568 patients (274 treated with chemo-endocrine therapy, 294 treated with endocrine therapy alone; 139 premenopausal, 429 postmenopausal). The primary endpoint of the substudy was the mean cognitive function score by treatment arm and menopausal status. Dr Irene Kang (City of Hope Orange County, CA, United States) presented the results [3].
In premenopausal participants treated with endocrine therapy alone, mean cognitive function score temporarily decreased after randomisation and returned to baseline value by 36 months. In contrast, in premenopausal patients treated with chemo-endocrine therapy the score decreased after randomisation and did not return to baseline value. The difference in longitudinal mean score between treatment arms (-3.02) was both statistically significant and clinically meaningful.
In postmenopausal participants treated with endocrine therapy alone, mean cognitive function score stayed stable during follow-up while in postmenopausal participants treated with chemo-endocrine therapy the score decreased after randomisation and did not return to baseline value. The difference in longitudinal mean score between treatment arms (-2.36) was statistically significant but not clinically meaningful.
The change in cognitive function was however heterogeneous. In both treatment groups and in both pre- and postmenopausal participants, most did not show a clinically meaningful worsening of cognitive function score during follow-up. Their score kept stable or was (clinically meaningful) better during follow-up. The odds of having worse cognitive function was highest in postmenopausal participants treated with chemo-endocrine therapy at 12 months after randomisation (OR 2.24; 95% CI 1.40–3.59).
“Chemo-endocrine therapy has a greater negative effect on cancer-related cognitive impairment compared with endocrine therapy alone both in pre- and postmenopausal women,” concluded Dr Kang. “In addition, the effect of chemo-endocrine therapy seems to persist over time in a significant portion of patients.”
- Ahles TA, et al. J Clin Oncol. 2012;30:3675–3686.
- Whittaker A, et al. Sci Rep. 2022;12:2135.
- Kang I, et al. Patient-reported cognitive impairment in women participating in the RxPONDERR trial (SWOG S1007) by menopausal status. Abstract GS1-04, SABCS 2022, 6–10 December, San Antonio, TX, USA.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
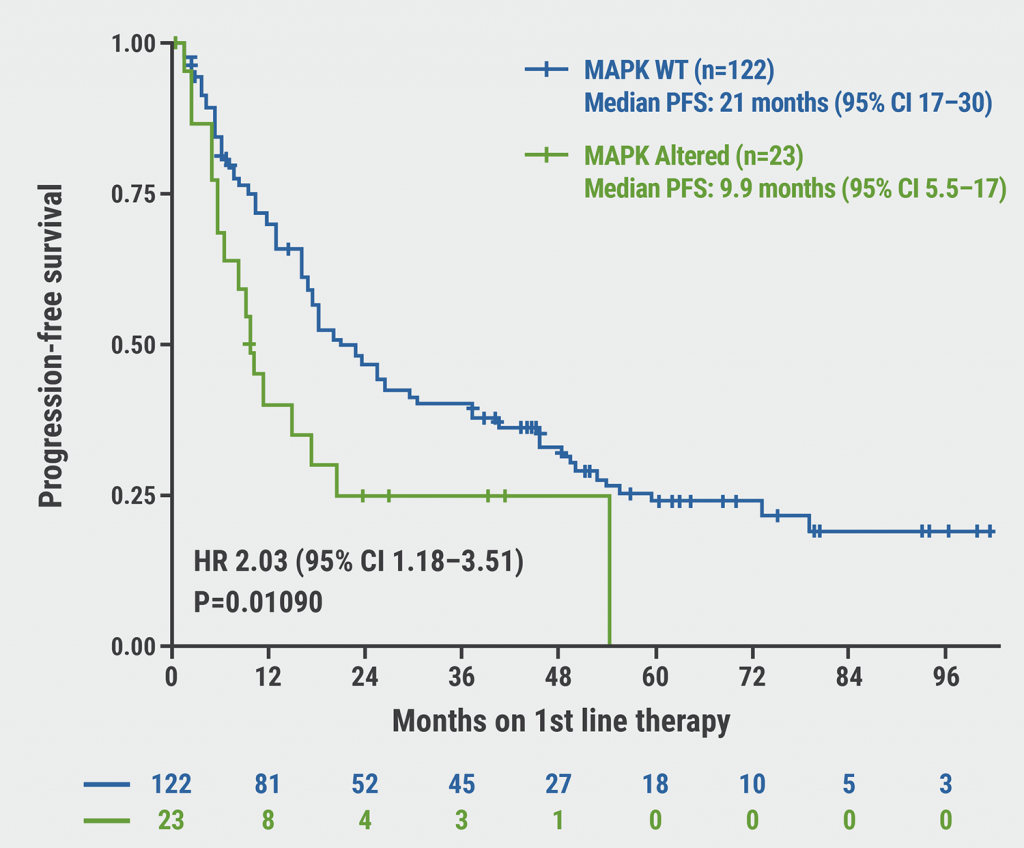
« Resistance to CDK4/6 inhibitors is likely due to expansion of pre-existing resistant clones Next Article
Racial disparity in the tumour microenvironment »
« Resistance to CDK4/6 inhibitors is likely due to expansion of pre-existing resistant clones Next Article
Racial disparity in the tumour microenvironment »
Table of Contents: SABCS 2022
Featured articles
Miscellaneous
Racial disparity in the tumour microenvironment
Chemo-endocrine therapy worse for cognition than endocrine therapy alone
Early-Stage Breast Cancer
Anti-PD-1/anti-LAG-3 combination highly effective in HER2-negative breast cancer
MammaPrint test predictive for benefit of extended endocrine therapy
HR-positive/HER2-positive Breast Cancer: Trastuzumab-Deruxtecan
Trastuzumab deruxtecan effective in both second-line and neoadjuvant setting
HR-positive/HER2-negative Advanced Metastatic Breast Cancer
Benefit of adjuvant abemaciclib continues to deepen at longer follow-up
First-line ribociclib plus endocrine therapy outperforms combination chemotherapy
Treatment options beyond CDK4/6 inhibition
Triple-Negative Breast Cancer
Baseline CTC count can guide first-line treatment in HR-positive/HER-negative metastatic breast cancer
ZNF689 deficiency promotes intratumour heterogeneity and resistance to immune checkpoint blockade in TNBC
Oestradiol represses anti-tumoural immune response to promote progression of brain metastases
Basic and Translational Research
Resistance to CDK4/6 inhibitors is likely due to expansion of pre-existing resistant clones
Germline pathogenic variants for breast cancer also increase contralateral breast cancer risk
Low-dose tamoxifen still prevents recurrence from non-invasive breast cancer
Endocrine interruption to pursue pregnancy does not impact short-term disease in breast cancer
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com