The CAPTIVATE trial investigated an ibrutinib plus venetoclax regimen in patients with CLL, divided in a fixed-duration cohort and a MRD cohort. Patients received 3 cycles of oral ibrutinib (420mg, daily), followed by 12 cycles of ibrutinib plus oral venetoclax (ramp-up to 400mg daily). The 2-year follow up results of the MRD-guided cohort were presented at the ASH annual meeting. During week 16, patients with confirmed uMRD were randomised 1:1 to placebo (n=43) or ibrutinib monotherapy (n=43). Patients who did not achieve uMRD were randomised 1:1 to ibrutinib monotherapy (n=31) or ibrutinib plus venetoclax therapy (n=32). Notably, a high proportion of patients had high-risk features, such as unmutated immunoglobulin heavy-chain variable region gene (IGHV) (60%). The median post-randomisation follow-up was 24 months.
With this longer follow-up, no new disease-free survival (DFS) events had occurred since the primary analysis in patients with confirmed uMRD. The DFS rates remained at 95% and 100% for placebo receivers and ibrutinib receivers, respectively. In addition, the overall study period displayed modest improvements in complete response (CR) rates for patients with confirmed uMRD, compared to the pre-randomisation period (placebo 9%, ibrutinib 5%). Patients without confirmed uMRD showed larger improvements in CR rates, with ibrutinib receivers displaying a 22% improvement and ibrutinib plus venetoclax receivers demonstrating a 28% improvement. Importantly, no new safety issues of the ibrutinib plus venetoclax regimen were observed.
Medicom interviewed Prof. Ghia to understand the context of these results.

Medicom: Do these data have the potential to alter the therapeutic landscape for CLL?
At ASH this year, I presented the CAPTIVATE study, which is a phase 2 study enrolling patients with the chronic lymphocytic leukaemia and treated in first line with a combination of ibrutinib plus venetoclax plus for 12 months, proceeded by three months of monotherapy with ibrutinib. The study includes two different cohorts, one fixed duration cohort, where all patients stopped the treatment at the end of the 12 months of combination, and the MRD cohort, which is the one that I presented here at ASH, where patients at the end of the 12 months of the combination, are randomised based on their MRD status.
In the MRD-guided cohort, those who achieved undetectable MRD were subsequently randomised to either discontinue treatments, so to the placebo arm, or to continue ibrutinib. On the other hand, the patients who did not achieve undetectable MRD were randomised to continue either ibrutinib alone, or ibrutinib plus venetoclax. What I presented at ASH was the two-year follow-up of this study.
We set the endpoint to be disease-free survival, which is an important distinction from progression free survival (PFS), because disease-free survival is a much more stringent endpoint. This endpoint considers the freedom from disease progression, obviously freedom from death, but also freedom from MRD relapse. Interestingly enough, with an extra year of follow-up, not a single additional event occurred, which is of course excellent for the patients.
Thus, the disease-free survival continues to remain above 95% in both arms, whether patients were treated with placebo (discontinued the treatment), and patients treated with ibrutinib. These data strongly confirm the notion that one might safely discontinue therapy when achieving undetectable MRD. We also presented the PFS update, nearly 3-year PFS progression-free survival for all patients enrolled in this cohort, as well as for the patients who did not achieve undetectable MRD and continued to be treated with either ibrutinib or ibrutinib plus venetoclax. Altogether, in all different arms of patients, the PFS was > 95%.
The main implication these data suggest is that if we tailor the treatment of patients based on MRD level, we can achieve a very good outcome in all patients, regardless of whether MRD was fully achieved in the initial treatment with a combination of drugs. However, despite the fact that we are talking about more than 95% of the patients doing very well, some patients did relapse, did progress, including some who had achieved MRD. Going forward, we will have to rigorously study what happens to these patients, and figure out how we can salvage their disease. We know that by design in this study, the patients who relapsed after placebo, of course, could be retreated with the ibrutinib or if they relapsed early that they could be retreated with a combination of ibrutinib plus venetoclax if they relapsed later. The patients who progress on ibrutinib alone can add venetoclax. Of course, the patients who progress on ibrutinib plus venetoclax will require another targeted therapy.
In particular, we are interested in is also to define the optimal patient selection, for example the genetic features of these patients so that we can predict those who will not benefit from the combination of treatment in the long run.
Medicom: The patient ages were relatively low, do you think these data will hold up in older patients?
Indeed, the patients enrolled in CAPTIVATE were typically young patients, even younger than a usual, with a median age of 50-51 years. Although our data therefore applies to young and fit patients, it is important to note that similar data have been also obtained in another study that has been presented at ASH: the GLOW study (NCT03462719). In GLOW, the same combination of 12 months of ibrutinib plus venetoclax, preceded by 3 months of ibrutinib, was compared with chlorambucil plus obinutuzumab. The difference is that this study was in first-line elderly patients, where indeed the chlorambucil plus obinutuzumab was still the standard immunochemotherapeutic treatment, and was the comparator. Confirming the data from CAPTIVATE, the patients in GLOW treated with ibrutinib plus venetoclax obtained a similar depth of response comparable to CAPTIVATE.
Medicom: The vast majority of patients was able to achieve the total treatment regimen, what does that say about tolerability and safety?
These data from the 2 studies strongly indicate that there is not much of a difference in efficacy based on the age of the patient. What is probably the difference that many more patients in the GLOW study had to discontinue the therapy or had to reduce the treatment and, in particular, they had more adverse events, in particular, grade 3 and 4 adverse events. In particular, infection was a concern. In fact, in the CAPTIVATE study, roughly 35% of patients had neutropenia, but only 8% had infections, which is very reasonable. In the GLOW study, a similar proportion of patients had neutropenia, but roughly double the patients had an infection. This may lead some physicians to think that ibrutinib plus venetoclax can be a very good option in particular for younger and fit patients, but also for elderly fit patients, but with careful monitoring for infections.
Admittedly, there will never be a one-size-fits-all treatment, but this is a great start. Probably some patients, in particular, the very old patients can still benefit from continuous monotherapy with BTK inhibitors. These data with ibrutinib plus venetoclax, however, do appear to tout extraordinary tolerability profiles, and very reasonable safety signals, mostly mild and easy to manage.
Reference
- Ghia P, et al. First-Line Treatment with Ibrutinib (Ibr) Plus Venetoclax (Ven) for Chronic Lymphocytic Leukemia (CLL): 2-year Post-Randomization Disease-Free Survival (DFS) Results from the Minimal Residual Disease (MRD) Cohort of the Phase 2 Captivate Study. Session 642, ASH 2021 Annual Meeting & Exposition, 11-14 December.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Spore therapy cuts C. difficile reinfection by 68% in 8-week study Next Article
Simple screening tools could help identify COPD in low-, middle-income countries »
« Spore therapy cuts C. difficile reinfection by 68% in 8-week study Next Article
Simple screening tools could help identify COPD in low-, middle-income countries »
Related Articles
September 9, 2020
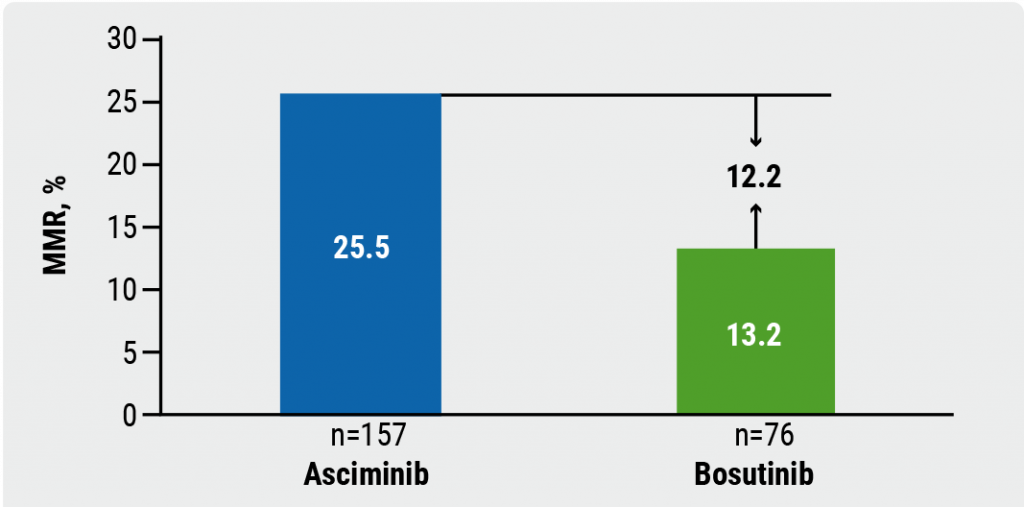
Asciminib monotherapy in Ph+ CML: major molecular responses
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

