Researchers examined administrative claims data on 57,220 adults who received a total of 752,150 biologic infusions for immune-mediated disease between 2007 and 2017. The analysis included a total of 34,078 (4.5%) home infusions for 3,954 patients as well as 718,072 (95.5%) facility infusions for 54,770 patients.
Compared to facility infusions, home infusions were associated with a significantly higher risk of an emergency department visit or hospital admission on the day of infusion or the following day (odds ratio 1.25).
Home infusions were also associated with a significantly greater chance that patients would discontinue treatment after an emergency department visit or hospital admission (OR 1.28).
"In an infusion center or office setting, biologic infusions are overseen by trained physicians with experience and resources for managing side effects and complications, which is typically not the case when biologic infusions are administered at home," said lead study author Dr. Matthew Baker, clinical chief for the Division of Immunology and Rheumatology in the Department of Medicine at Stanford University in California.
When issues arise in the home setting, there may be a lower threshold for escalation of care, Dr. Baker said by email.
"Thus, it is not surprising that we found an increased risk of emergency department visit or hospital admission within 24 hours of home infusions compared to facility infusions," Dr. Baker said.
There were some key differences between patients who had home infusions. For example, they were younger (mean age 43.2) years than patients who got facility infusions (mean age 51.3 years). And they were also more likely to be male (41%) than patients who got facility infusions (31.4%).
The proportion of home infusions resulting in emergency department visits and hospital admissions was highest after the first biologic infusion at home (4.9%), then dropped with the second infusion (4.3%) and third infusion (3.9%) of the same medicine.
Researchers didn't find any difference in post-infusion mortality between home- and facility-administered infusions.
One limitation of the claims data analysis is that there may be a potential for residual or unmeasured confounders to influence the outcomes, the study team notes in JAMA Network Open. Researchers also lacked data on disease modifying medications such as methotrexate as well as other medications that might have influenced the risk of adverse events with infusions.
"It's difficult to know for certain if the adverse events were directly associated with the biologic infusion," said Gregory Calip, a senior quantitative scientist at Flatiron Health in New York City and co-author of a commentary accompanying the study.
Other factors - like access to urgent care, co-medications, and ability to monitor for mild infusion reactions that may not necessarily require emergency department or hospital visits if administered at a facility - could all affect the likelihood of patients seeking acute care, Calip said by email.
"It is possible that some adverse events occurring at a facility that has resources to immediately address them are resolved early, without the need for an emergency department visit or hospitalization," Calip added.
SOURCE: https://bit.ly/3ziD1WQ and https://bit.ly/3zhreIm JAMA Network Open, online June 3, 2021.
By Lisa Rapaport
Posted on
Previous Article
« Maternal antiseizure medication not tied to adverse outcomes in offspring Next Article
ANALYSIS-U.S. FDA faces mounting criticism over Alzheimer’s drug approval »
« Maternal antiseizure medication not tied to adverse outcomes in offspring Next Article
ANALYSIS-U.S. FDA faces mounting criticism over Alzheimer’s drug approval »
Related Articles
September 17, 2021
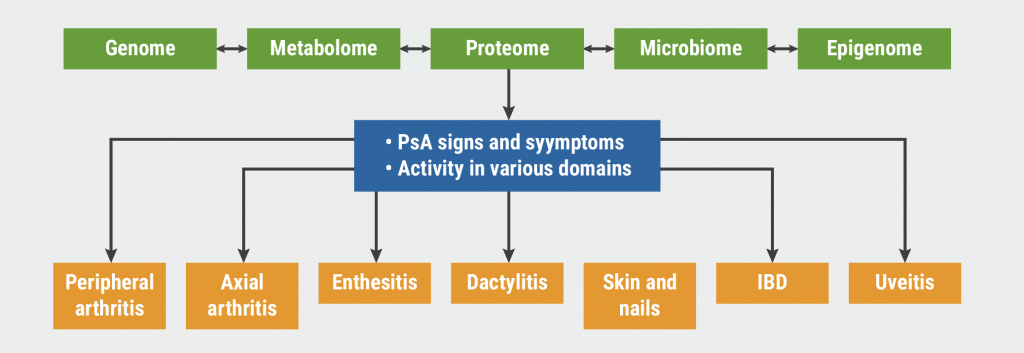
Psoriatic arthritis: Guidelines and best practice
January 18, 2021
Promising novel treatment option for psoriatic arthritis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

