https://doi.org/10.55788/bbffe179
Anti-Ro/SSA antibodies have been associated with interstitial lung disease (ILD) in different connective tissue diseases [1,2]. Yet, despite better stratification of SSc patients with SSc-specific antibodies, individual prognosis remains unpredictable [3]. Thus, further exploration of SSc non-specific antibodies is crucial to enhance risk assessment and refine management strategies for SSc patients.
Dr Blaž Burja (University Hospital Zurich, Switzerland) and his team evaluated the prevalence of anti-Ro/SSA antibodies in patients with SSc and the association of these antibodies with disease phenotype and clinical outcomes, focussing on lung involvement [4]. “We examined the largest available cohort of established SSc patients selected from the EUSTAR database together with available data on anti-Ro/SSA antibodies,” Dr Burja explained.
The team assessed the presence of lung fibrosis using high-resolution computer tomography (HRCT) over a median of 2.7 years of follow-up, employing multivariable logistic regression to identify associated factors. In addition, the impact of anti-Ro/SSA antibodies on lung function (i.e. functional vital capacity [FVC] and diffusing capacity for carbon monoxide [DLCO]) in these patients was calculated.
Out of 4,421 patients with SSc meeting the 2013 criteria in the EUSTAR database, 661 (15.2%) tested positive for anti-Ro/SSA antibodies. These antibodies were significantly linked (P<0.001) with anti-SSB, anti-U1RNP antibodies, and rheumatoid factor. Patients with anti-Ro/SSA antibodies showed higher rates of muscular involvement (18% vs 12.5%; P<0.001) and ILD (56.2% vs 47.8%; P=0.001) compared with those without. The presence of anti-Ro/SSA antibodies independently predicted the presence of lung fibrosis during follow-up (OR 1.24; 95% CI 1.07–1.44; P=0.006; see Figure) and was associated with lower DLCO (regression coefficient -1.93; 95% CI -3.83 to 0.02; P=0.049) in affected patients. Also, it revealed a trend for lower FVC in these individuals (P=0.082). However, anti-Ro/SSA antibodies did not predict the progression of lung fibrosis or mortality over time.
Figure: Anti-Ro/SSA antibodies are a risk factor for ILD [4]

ANA, antinuclear antibodies; CRP, C-reactive protein; GI, gastrointestinal; ILD, interstitial lung disease; LVEF, left ventricular ejection fraction; SSc, systemic sclerosis.
Multivariable analysis from 14,066 visits; adjusted for known risk factors for ILD.
“Overall, the presence of anti-Ro/SSA antibodies in 15.2% of the SSc cohort signifies an independent risk factor for lung fibrosis development,” Dr Burja concluded. Therefore, integrating the assessment of anti-Ro/SSA antibodies into routine clinical practice is advisable to identify individuals at higher risk of ILD, particularly beneficial in settings without access to HRCT scans, where these antibodies can serve as crucial biomarkers for screening.
- Wodkowsky M, et al. Clin Exp Rheum 2015;33 (Suppl. 91):S131-135.
- Nagy A, et al. Front Pharmacol 2021;12:778649.
- Elhai M, et al. Lancet Rheumatol 2022;4:E785-794.
- Burja B, et al. Anti-Ro/SSA antibodies are predictive of a more severe lung involvement in patients with systemic sclerosis: a study from the EUSTAR database. OP0013, EULAR 2024 Congress, 12–15 June, Vienna, Austria.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« Early treatment with ambrisentan might prevent PAH development in patients with SSc Next Article
Daratumumab shows promise in systemic lupus erythematosus »
« Early treatment with ambrisentan might prevent PAH development in patients with SSc Next Article
Daratumumab shows promise in systemic lupus erythematosus »
Table of Contents: EULAR 2024
Featured articles
Advanced therapies show promising results in PsA real-world study
Small protein targeting IL-17A effective in PsA management
Late-breaking Abstracts
Nipocalimab meets primary endpoint in Sjögren’s syndrome
Advanced therapies show promising results in PsA real-world study
Dual IL-17A/F blocker significantly reduces spinal radiographic progression in radiographic axSpA
Small protein targeting IL-17A effective in PsA management
Spotlight on Rheumatoid Arthritis
New JAK1 inhibitor outperforms placebo in active RA
Macrophage profiling in synovial tissue predicts treatment response in RA
Innovative app boosts mental health in patients with RA
What is New in Lupus and Scleroderma
Daratumumab shows promise in systemic lupus erythematosus
Severe lung involvement in SSc linked to anti-Ro/SSA antibodies
Early treatment with ambrisentan might prevent PAH development in patients with SSc
Crystal-related Disorders in 2024
More patients hit their uric acid target with febuxostat and ruzinurad combination
Tophaceous gout at higher mortality risk than non-tophaceous gout
JAK Inhibition in Giant Cell Arteritis
Is JAK inhibition the right choice for patients with relapsing giant cell arteritis?
Giant cell arteritis: Upadacitinib may be an upcoming treatment option
Spotlight on Other Indications
AxSpA: Higher comorbidity burden worsens radiographic progression
Hope for a durable effective injection therapy in knee osteoarthritis
Dermatomyositis: Triple therapy with tacrolimus beats cyclosporin regimen
Best of the Posters
Less fracture risk with denosumab than bisphosphonates in pre-treated osteoporosis
Low IL-18: a hidden culprit of long COVID in patients with autoimmune disease
Stopping DMARDs? These key factors predict RA flares
Related Articles
September 4, 2019
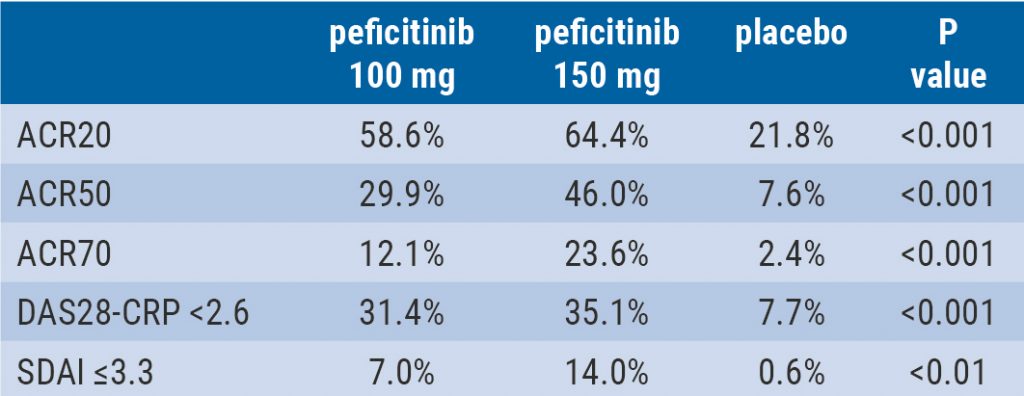
Peficitinib likely efficacious and safe
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

