https://doi.org/10.55788/68acdacb
“What we always wanted to know is how bimekizumab modifies disease progression but also radiographic progression in terms of clinical data,” explained Prof. Xenofon Baraliakos (Ruhr-University Bochum, Germany) [1]. To answer this question, the ongoing OLE (NCT04436640) of the phase 3 BE MOBILE 2 study (NCT03928743) assesses the impact of bimekizumab on spinal radiographic progression over 164 weeks. Prof. Baraliakos presented the interim analysis at week 104. “We need at least 2 years of follow-up to assess radiographic changes,” Prof. Baraliakos explained.
The BE MOBILE 2 study involved 332 participants, 286 of whom entered the OLE, and 267 completed the 104 weeks. The participants received bimekizumab 160 mg subcutaneously every 4 weeks. “Because damage at the beginning is the most important factor for disease progression, we assessed it at baseline,” Prof. Baraliakos said. Baseline modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS) was relatively high at 7.3. Radiographs were repeated at week 104, with progression independently assessed by 2 central readers using the mSASSS (range 0–72).
At 2 years, the results showed only minimal spinal radiographic progression in participants treated with bimekizumab. The mean mSASSS change from baseline was 0.3. No radiographic progression was shown by 85.3% of the participants (mSASSS change ≤0.5), and 92.1% showed less than 2 points increase in mSASSS. Moreover, non-progressors at week 104 included 83.1% of the participants with pre-existing structural damage.
No significant predictive factors for spinal radiographic progression were identified, including baseline mSASSS, age, sex, BMI, ethnicity, smoking status, baseline Ankylosing Spondylitis Disease Activity Score (ASDAS), baseline high-sensitivity C-reactive protein level, prior TNF inhibitor use, and ASDAS and Assessment in SpondyloArthritis international Society 40% (ASAS40) response at week 104.
Only a fraction of participants had new syndesmophytes at 2 years of bimekizumab treatment, including almost one-fifth who had existing syndesmophytes at baseline. This shows that participants with syndesmophytes at baseline are particularly prone to progress. Safety data indicated that bimekizumab was well-tolerated, with no unexpected adverse events reported.
Prof. Baraliakos concluded that the high proportion of participants maintaining a ‘non-progression’ status over 2 years in this study supports the use and further investigation of bimekizumab as a viable long-term treatment option for axSpA.
- Baraliakos X. et al. Minimal spinal radiographic progression in patients with radiographic axial spondyloarthritis over 2 years of bimekizumab treatment: Results from a phase 3 open-label extension study. LBA0003, EULAR 2024 Congress, 12–15 June, Vienna, Austria.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« Small protein targeting IL-17A effective in PsA management Next Article
Advanced therapies show promising results in PsA real-world study »
« Small protein targeting IL-17A effective in PsA management Next Article
Advanced therapies show promising results in PsA real-world study »
Table of Contents: EULAR 2024
Featured articles
Advanced therapies show promising results in PsA real-world study
Small protein targeting IL-17A effective in PsA management
Late-breaking Abstracts
Nipocalimab meets primary endpoint in Sjögren’s syndrome
Advanced therapies show promising results in PsA real-world study
Dual IL-17A/F blocker significantly reduces spinal radiographic progression in radiographic axSpA
Small protein targeting IL-17A effective in PsA management
Spotlight on Rheumatoid Arthritis
New JAK1 inhibitor outperforms placebo in active RA
Macrophage profiling in synovial tissue predicts treatment response in RA
Innovative app boosts mental health in patients with RA
What is New in Lupus and Scleroderma
Daratumumab shows promise in systemic lupus erythematosus
Severe lung involvement in SSc linked to anti-Ro/SSA antibodies
Early treatment with ambrisentan might prevent PAH development in patients with SSc
Crystal-related Disorders in 2024
More patients hit their uric acid target with febuxostat and ruzinurad combination
Tophaceous gout at higher mortality risk than non-tophaceous gout
JAK Inhibition in Giant Cell Arteritis
Is JAK inhibition the right choice for patients with relapsing giant cell arteritis?
Giant cell arteritis: Upadacitinib may be an upcoming treatment option
Spotlight on Other Indications
AxSpA: Higher comorbidity burden worsens radiographic progression
Hope for a durable effective injection therapy in knee osteoarthritis
Dermatomyositis: Triple therapy with tacrolimus beats cyclosporin regimen
Best of the Posters
Less fracture risk with denosumab than bisphosphonates in pre-treated osteoporosis
Low IL-18: a hidden culprit of long COVID in patients with autoimmune disease
Stopping DMARDs? These key factors predict RA flares
Related Articles
August 2, 2021
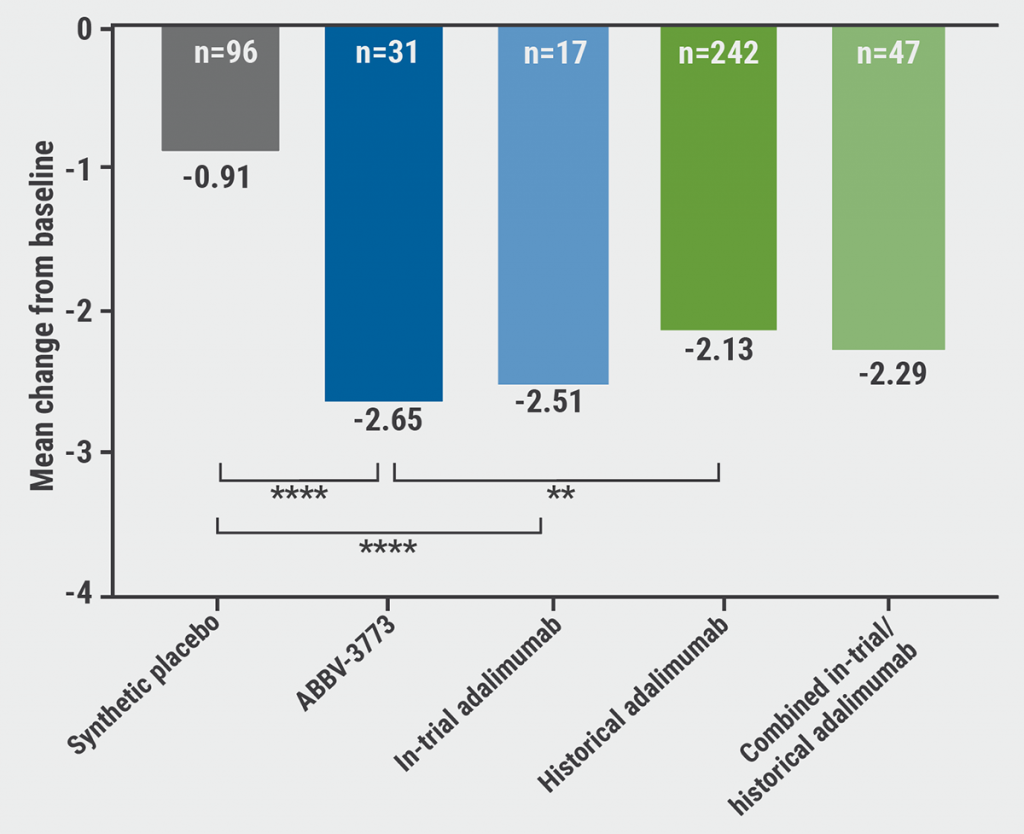
ABBV-3373: A potential new therapeutic agent for RA
August 14, 2020
New nanoparticle promising future agent in RA
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

