https://doi.org/10.55788/3e6bb009
EUSTAR was launched in 2004, aiming to unify research efforts in the field of SSc. This EUSTAR analysis aimed to estimate the annual incidence of ILD in SSc patients and identify risk factors for new-onset ILD. Dr Liubov Petelytska (Bogomolets National Medical University, Kyiv, Ukraine) presented the results.
Of 23,195 SSc patients from the EUSTAR dataset, 11,501 had an available ILD status on HRCT, the gold standard for diagnosing SSc-ILD. At baseline, just over half (n=6,270) were ILD-positive (incident group), while 5,331 did not have ILD (at-risk group). Incidence was calculated as the rate per 100 person-years, starting from the first hospital visit.
Results showed that new-onset ILD occurred in 1,075 (20.2%) patients in the at-risk group after a median follow-up of 3.8 years. Surprisingly, the incidence of new-onset ILD was independent of disease duration. Overall incidence was 3.83 per 100 person-years and was found to occur anytime during a 10-year observation period. Among other variables, the following factors were found to predictive of ILD in the long term: age (HR 1.0; 95% CI 1. –1.02), male sex (HR 1.4; 95% CI 1.1–1.8), history of arthritis (HR 0.7; 95% CI 0.5–0.9), dyspnea NYHA stage≥2 (HR 1.4; 95% CI 1.1–1.7), anti-topoisomerase antibody positivity (HR 2.4; 95% CI 2.0–2.8), anti-centromere antibody positivity (HR 0.7; 95% CI 0.6–0.8), PM/Scl autoantibody positivity (HR 2.0; 95% CI 1.2–3.6), inflammatory markers (HR 1.4; 95% CI 1.2–1.7), number of HRCTs during FU (HR 0.5; 95% CI 0.5–0.5), and average time between HRCTs (HR 3.2; 95% CI 2.8–3.6).
The study had several limitations, such as the heterogeneity of the population, the limited number of patients (50%) who had a follow-up HRCT available, and the use of registry data with missing values and decentralised reading.
- Petelytska L, et al. Incidence and risk factors for new onset of interstitial lung disease in systemic sclerosis: a EUSTAR analysis. 1700, ACR Convergence 2023, 10–15 November, San Diego, USA.
Medical writing support was provided by Michiel Tent.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« Novel selective URAT1 inhibitor shows promise in gout Next Article
Encouraging results of afimetoran in participants with cutaneous lupus »
« Novel selective URAT1 inhibitor shows promise in gout Next Article
Encouraging results of afimetoran in participants with cutaneous lupus »
Table of Contents: ACR 2023
Featured articles
Ixekizumab resolves nail psoriasis better than adalimumab in PsA
IV secukinumab safe and effective for long-term treatment of active PsA
Rheumatoid Arthritis
Short-term glucocorticoid use increases the risk of MACE
Positive efficacy and safety results of novel BlyS/APRIL inhibitor in RA
Baricitinib superior to TNFi in patients with RA who failed csDMARDs
Lupus
Encouraging results of afimetoran in participants with cutaneous lupus
CAR-T cell therapy results in sustained lupus remission
Osteoarthritis
Repeat steroid injection in knee osteoarthritis possibly beneficial
Osteoporosis
Romosozumab tops denosumab in glucocorticoid users with high fracture risk
Psoriatic Arthritis
Ixekizumab resolves nail psoriasis better than adalimumab in PsA
IV secukinumab safe and effective for long-term treatment of active PsA
Apremilast in early oligoarticular PsA: phase 4 study results
Gout
Novel selective URAT1 inhibitor shows promise in gout
Fibrosing rheumatic diseases
Incidence and risk factors for new-onset interstitial lung disease
No need to avoid TNF inhibitors in RA-ILD?
Vasculitis
Reduced-dose glucocorticoids in GPA and MPA increase mortality
Related Articles
February 26, 2024
Join the conversation on Rare Disease Awareness Day
February 4, 2020
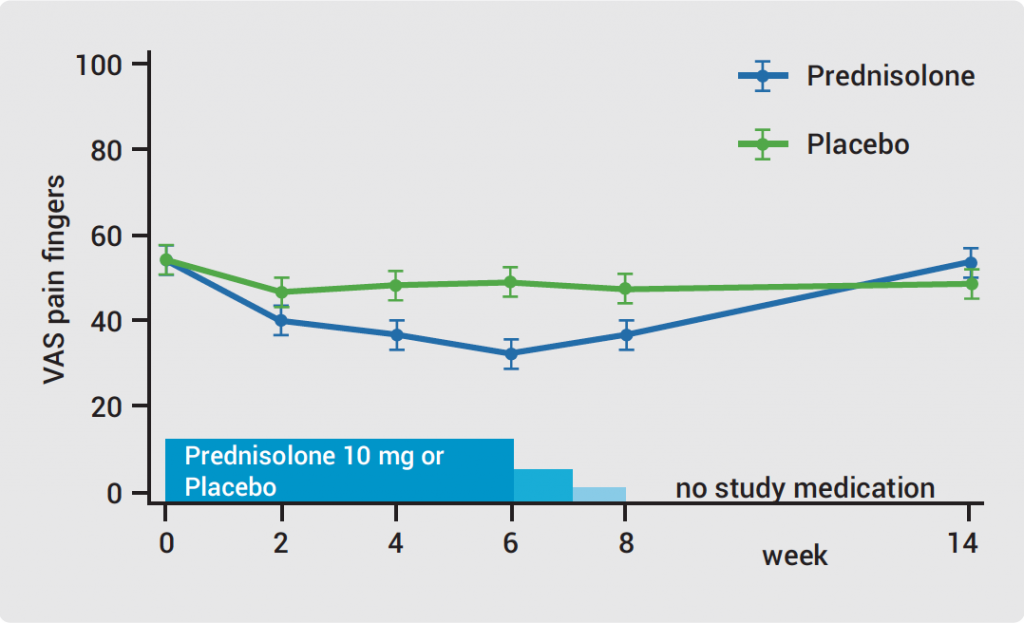
Hand OA: low-dose corticosteroids improve symptoms
September 17, 2021
Bridging the gap between patients and access to psoriasis specialists
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

