https://doi.org/10.55788/8f491398
A distinct unmet need exists for CLE therapies: it has been over 50 years since the last therapy was approved. Afimetoran is a first-in-class inhibitor of TLR7/8. A phase 1b study (NCT04493541) investigated the safety, tolerability, and exploratory efficacy of afimetoran in participants with CLE [1]. The results were presented by Dr Fareeda Hosein (Bristol Myers Squibb, NJ, USA).
Participants were aged 18–65, diagnosed with either SLE or had biopsy-proven CLE, had a modified CLE Disease Area and Severity Index-Activity (CLASI-A) score of ≥6, and were antinuclear antibody positive. They could use oral corticosteroids and/or antimalarials at baseline. The 13 participants were randomised 2:1 to once-daily oral afimetoran 30 mg (n=8) or placebo (n=5) for 16 weeks. The primary endpoints were safety and tolerability, while efficacy was exploratory.
Afimetoran demonstrated a favourable safety profile and was well tolerated. There were no serious adverse events (AEs) or safety signals in any participant. In the experimental arm, 1 participant discontinued treatment due to a symptomatic COVID-19 infection. The number of participants with AEs was 5 (63%) in the afimetoran group and 4 (80%) in the control group. These AEs were mild or moderate and resolved without intervention. Plasma concentrations exceeded the projected targeted inhibition concentration over 24 hours, supporting the 30 mg once-daily dosing.
The exploratory efficacy response was in line with the pharmacodynamic effects. Participants in the treatment group showed a greater reduction in CLASI-A scores as early as week 4 compared with placebo. By week 16, the rate of participants achieving the minimum clinically important difference in CLASI-A scores (>4 points from baseline) was higher for afimetoran (50%) than placebo (0%).
- Hosein A, et al. Safety, tolerability, and exploratory efficacy of afimetoran, a TLR7/8 inhibitor, in patients with cutaneous lupus erythematosus: A phase 1B randomized, double-blind, placebo-controlled study. L17, ACR Convergence 2023, 10–15 November, San Diego, USA.
Medical writing support was provided by Michiel Tent.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« Incidence and risk factors for new-onset interstitial lung disease Next Article
Positive efficacy and safety results of novel BlyS/APRIL inhibitor in RA »
« Incidence and risk factors for new-onset interstitial lung disease Next Article
Positive efficacy and safety results of novel BlyS/APRIL inhibitor in RA »
Table of Contents: ACR 2023
Featured articles
Ixekizumab resolves nail psoriasis better than adalimumab in PsA
IV secukinumab safe and effective for long-term treatment of active PsA
Rheumatoid Arthritis
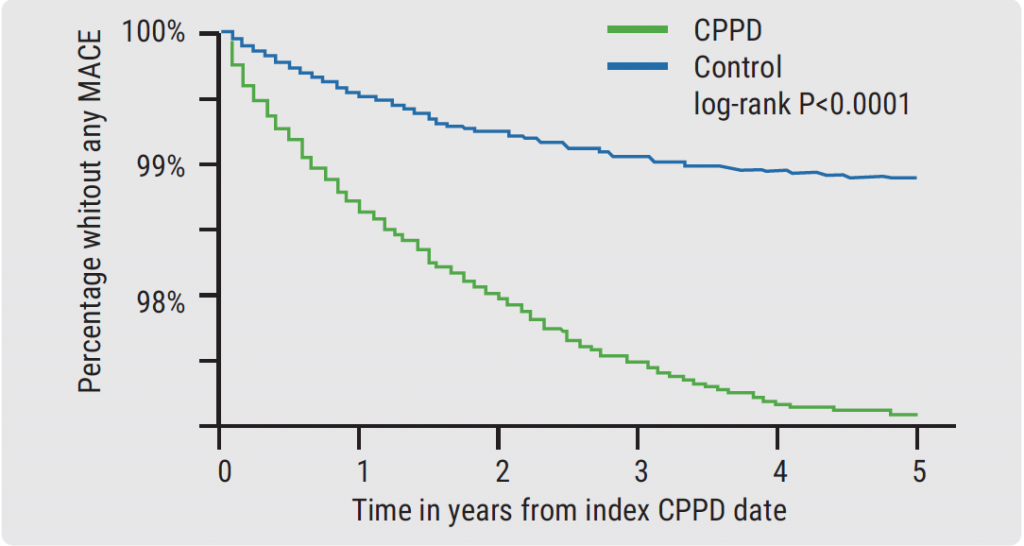
Short-term glucocorticoid use increases the risk of MACE
Positive efficacy and safety results of novel BlyS/APRIL inhibitor in RA
Baricitinib superior to TNFi in patients with RA who failed csDMARDs
Lupus
Encouraging results of afimetoran in participants with cutaneous lupus
CAR-T cell therapy results in sustained lupus remission
Osteoarthritis
Repeat steroid injection in knee osteoarthritis possibly beneficial
Osteoporosis
Romosozumab tops denosumab in glucocorticoid users with high fracture risk
Psoriatic Arthritis
Ixekizumab resolves nail psoriasis better than adalimumab in PsA
IV secukinumab safe and effective for long-term treatment of active PsA
Apremilast in early oligoarticular PsA: phase 4 study results
Gout
Novel selective URAT1 inhibitor shows promise in gout
Fibrosing rheumatic diseases
Incidence and risk factors for new-onset interstitial lung disease
No need to avoid TNF inhibitors in RA-ILD?
Vasculitis
Reduced-dose glucocorticoids in GPA and MPA increase mortality
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com