However, their real-world recommendations may differ based on the type of healthcare system they practice in, their years of experience, and the number of chest scans they review per week, the authors write in the Journal of the American College of Radiology.
"There appears to be a gap between self-reported adherence with nodule-evaluation guidelines and observed adherence in actual practice," said lead author Dr. Michael Gould of the Kaiser Permanente Bernard J. Tyson School of Medicine in Pasadena, California.
"Our data suggest that the gap is not due to limitations in radiologist awareness or agreement with the existing guidelines and that other factors need to be identified," he told Reuters Health by email.
Each year, more than 1.5 million Americans are diagnosed with incidental pulmonary nodules found on chest scans, Dr. Gould and his colleagues write. Most are benign, but about 5% are cancer-related.
Guidelines are continuously updated to help radiologists and pulmonologists assess the malignancy of nodules. The American College of Radiology and other groups suggest observing the nodules over time rather than taking a biopsy. However, studies have found that radiologists may differ in their practices, which could be based on a variety of factors, the authors write.
Dr. Gould and colleagues surveyed 127 radiologists in 13 healthcare systems participating in the Watch the Spot Trial, a comparative-effectiveness trial of guideline-based protocols for nodule surveillance in the U.S. The survey asked about radiologists' awareness, agreement and adherence to different guidelines, including ones from the Fleischner Society and the Lung CT Screening Reporting Data System, or Lung-RADS.
Overall, 95% of radiologists were familiar with the Fleischner guidelines, and 71% were familiar with the Lung-RADS guidelines. About 94% of the survey participants said they followed guidelines for nodules detected during lung-cancer screenings, and 97% said they followed guidelines for nodules detected incidentally during other chest scans.
The majority of radiologists said the benefits of following the guidelines outweighed the risks, and 70% said the frequency of follow-ups seemed "just right" for ongoing chest scans.
Most radiologists considered the scientific evidence underlying the guidelines to be of high quality, though it differed by type. About 68% thought the evidence for screening-detected nodules was high-quality, as compared with 41% for incidental nodules.
This varied by practice type, too. Nearly 80% of radiologists who practiced in nonintegrated healthcare systems said the underlying evidence was high-quality, as compared with 57% of those in integrated systems. Those who read 20 or fewer chest scans per week were less aware of the guidelines and less likely to follow them.
In addition to guidelines, nearly all of the radiologists said that other factors influence their recommendations for lung-nodule surveillance, including risk factors for lung cancer, protocols within their institution, the risk of litigation for a missed cancer diagnosis, and the potential harms of either under-evaluation or over-evaluation.
"We need more studies of nodule-evaluation strategies to determine the optimal frequency and duration of follow-up," Dr. Gould said. "In the meantime, it is reasonable to follow the Lung-RADS and Fleischner Society recommendations."
Location and practice setting likely contribute heavily to a radiologist's approach, said Dr. David Naidich of the New York University Medical Center. Dr. Naidich, who wasn't involved in the survey, has researched and written about lung-cancer screening and nodule guidelines.
"A radiologist's approach to interpreting anything is not done in a vacuum," he told Reuters Health by phone. "How another physician refers a scan for evaluation in the first place, and how that referring physician responds to the evaluation, is not trivial."
The causes of incidental nodules tend to vary based on geographic location in the U.S. as well, Dr. Gould said, which could influence how radiologists and referring physicians interpret results and report them to patients.
"Incidental nodules in Wisconsin and California are not the same creature," he said. "That's going to change how physicians look at those nodules and monitor them."
SOURCE: https://bit.ly/37E932o Journal of the American College of Radiology, online November 17, 2020.
By Carolyn Crist
Posted on
Previous Article
« EASD 2020 Highlights Podcast Next Article
Sequential IV ibandronate tied to BMD increase »
« EASD 2020 Highlights Podcast Next Article
Sequential IV ibandronate tied to BMD increase »
Related Articles

September 8, 2020
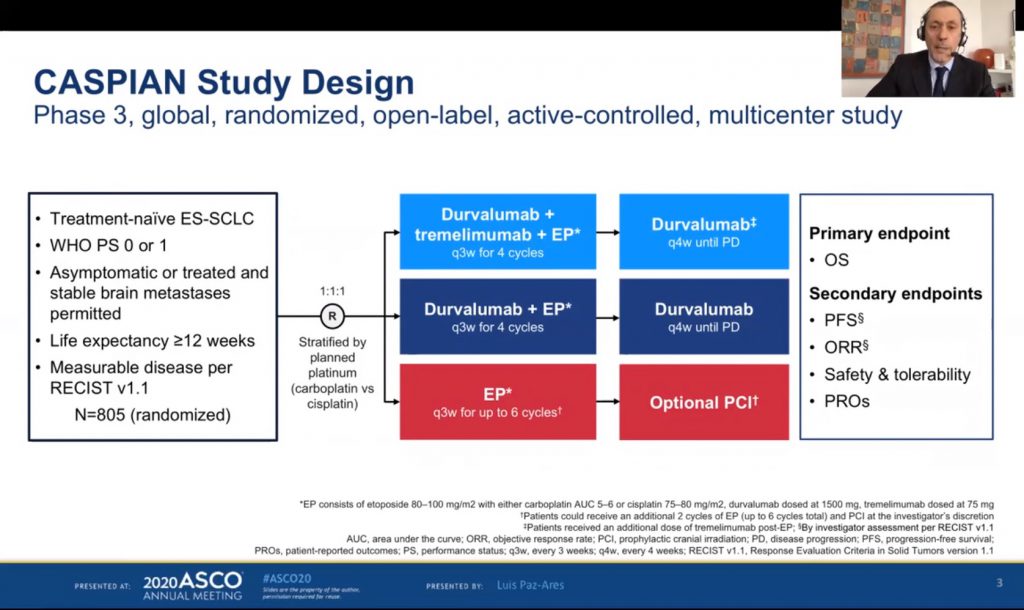
ES-SCLC: tremelimumab + durvalumab + chemotherapy misses endpoint
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

