October is Breast Cancer Awareness Month! The Know Your Lemons Foundation was founded in 2014 by Dr Corrine Ellsworth-Beaumont, a designer who lost her grandmothers and a close friend to breast cancer. She created the #knowyourlemons campaign as an initiative to help improve early detection of breast cancer through symptoms and screening education in a fun, accessible, and inclusive way.
October is Breast Cancer Awareness Month! The Know Your Lemons Foundation was founded in 2014 by Dr Corrine Ellsworth-Beaumont, a designer who lost her grandmothers and a close friend to breast cancer. She created the #knowyourlemons campaign as an initiative to help improve early detection of breast cancer through symptoms and screening education in a fun, accessible, and inclusive way.Medicom Medical Publishers interviewed Dr Corinne Ellsworth-Beaumont in Long Beach California, at the World Cancer Leaders’ Summit. Using 12 lemons instead of breasts helps the campaign achieve a global reach, overcoming cultural taboos around breasts.
What can you tell us about the #knowyourlemons campaign?
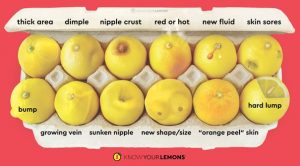
There are taboos around breasts and there's a real fear around the topic of cancer. When you combine those 2 things with breast cancer, it can make the topic very inaccessible to people and that's why it’s difficult to talk about breast health and breast cancer; those conversations never begin. In our campaign we use a lemon as a metaphor for the breast to visualise breast cancer symptoms. We’ve developed an image of 12 lemons in an egg box and each of those 12 lemons show a different symptom of breast cancer. That’s why the campaign is called #knowyourlemons, which is done under my charity, the Know Your Lemons Foundation. To date, we have reached 1.85 billion people online with the campaign in 34 languages, and it's helping educate people around the world.
People have said that seeing this image made all the difference in them being able to recognise that they had a breast change that could be a symptom of breast cancer. We make it easier for patients to understand the symptoms and feel more confident when they approach a doctor about their breast change. So often, especially younger women, will get dismissed by their doctor because the doctor isn't always aware of all the symptoms of breast cancer.
We developed an app called the Know Your Lemons app. It's currently available in four languages: English, French, Spanish, and German. The app teaches people how to do self-exams, what different breast anatomy feels like, for example, what does a lymph node feel like compared with a suspicious lump. And then there are monthly self-exam reminders given to patients.
If a woman thinks to have found something during their self-exam after using the audio guide, we have Mona Lisa to explain what each part of the breast feels like. With help from Mona Lisa we've had patients that were able to actually find a lump themselves and got diagnosed early. The other breast health coach is Napoleon. He's very good at examining the landscape of the breast, but he is for men, for women who have had mastectomies and for people who have had top surgery. This way we are absolutely inclusive in how we educate.
If the patient has any concerns after completing the self-exam, the app will take them to a list of all the symptoms and they can read about each one in detail. A patient guide will further explain how to have a conversation with their doctor and which kind of testing they should be referring for you. And, importantly, it is within a patient right to insist on testing for breast changes.
We also have our volunteer educator program where we train volunteers as "Lemonistas". They teach breast health classes in their communities. We started this program in 2020, and right now we have 800 trained volunteer educators in 60 countries and we've taught almost 100,000 people in person. On several occasions, people went to a class thinking "Oh, well, I'll learn something about breast health," and at the end of the class they realised, "Oh, so this thing I've noticed on my breast is something that should be investigated." They were able to get diagnosed earlier than if they had not had the education at all.
How can physicians, especially general practitioners, participate in this sort of education campaign?
We have a poster that physicians can put on the exam room door. The poster has a QR code for the app. But there are 3 things that can happen as a result of having this poster in the exam room.
- While patients are waiting in the exam room they will have time to look at the poster. Patients say it makes them curious and want to learn more. Some have said they would come in for another reason, but then see the poster and realise, "Oh, this is a breast issue that I have and need to talk to my doctor about." It great to help patients recognise a breast issue that they might not have realised before.
- Support staff like the physician's assistant can also use the poster after they do standard tests, like measuring a patient’s blood pressure. They can point to the poster before the patient leaves and say, "Make sure to have a look at this and download the app because you can do an assessment that will help you understand what screening plan you should be on based on your particular risk factors."When a patient takes the assessment, it produces a bullet point list of risk factors that relate to possibly adjusting a breast cancer screening plan. The physician can look at that bullet point list and suggest a patient starting mammograms at age 40, or recommend genetic testing if a patient has 2 members of their family that were diagnosed with breast before age 50.
- Finally, it's just an easy way to bring up the discussion without having to say breast or cancer. A doctor can just point to the poster at the end of the visit if none of this has been brought up and just say, “Make sure if you notice anything like this to let me know. And that's a really easy way to highlight breast health for the patient without adding extra time to their visit.
The posters are available in a variety of languages. You can order them at the Know Your Lemons shop. We have a variety of patient education materials in different languages that physicians can hand out, including materials for low-literacy audiences.
What are the sorts of educational materials that you generate?
With a company called Dandelion Health, we have created a toolkit for doctors and patients, the healthcare team and patients to make communicating a diagnosis much easier. Traditionally a diagnosis is communicated verbally and we know that verbal communication has a very low efficacy rate when it comes to accurate memory retention. But when visuals are introduced that memory retention actually increases significantly. Using visuals as part of the diagnostic conversation can really help patients better understand it, can mean the healthcare team is repeating themselves less often, and can make patients feel a little bit more in control when they are overwhelmed with so much information, especially at the beginning.
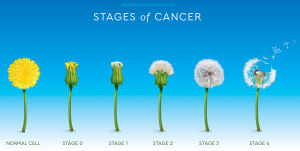
We use a dandelion as a metaphor to explain how cancer spreads. We have pictures of a dandelion in different stages, with stage four as the seeds being blown away to another location. We also use the dandelion to explain cancer pathology; using the dandelion seed as a metaphor, we illustrate that there are 2 parts to test for in breast cancer. One is to see if the cancer is using hormones to grow. The other part is to see if it's using proteins like HER2 to grow. Depending on what kind of dandelion seed you have, meaning what kind of subtype of breast cancer the patient has, there are different treatments that are going to be more effective than others.
The same way as you try to get rid of a dandelion in the grass there are similar approaches to cancer treatment. We illustrate the 6 different types of cancer treatment using a visual of a dandelion. This is explained with a conversation card that the oncologist would use to communicate the breast cancer diagnosis to the patient, with a lot of checkboxes and circling things, so it doesn't require a lot of writing. At home the patient would transfer the information from the conversation card to a small notebook which explains each of the concepts in further detail. While filling this out, the patient will recognise what parts of the conversation they understood and which parts of the conversation they're still not clear about. They're also going to see blank spaces in this notebook where conversations haven't happened yet. For example, has fertility been discussed with the patient? In this notebook we also explain about being wary of internet cures and well-intentioned relatives and friends that will pass on information to them.
Ideally this notebook enables the patient to know what they don't know, and how to bring up these topics with their doctor, rather than kind of blindly going into these additional conversations where the healthcare team says, do you have any questions and the patient's not really sure what vocabulary to use or how to ask. Instead of having to say endocrine therapy, a patient can point to a picture and say, “ I understand I'm supposed to have this treatment. Can you help me understand more about this and what I can expect?” It makes it much easier to facilitate conversations and have shared decision-making. Also, when patients are able to understand what their treatment is and why, adherence to treatment improves.
With our #knowyourlemons campaign and the educational materials we are trying to include more visuals in the way we talk and transfer knowledge to patients. This is an attempt to move away from the model of verbal communication only. I gave a TED Talk on this topic called Can an Image Save Lives from Cancer? It explains the process I went through developing these visuals and and the outcomes that have happened around the world as a result of using visual communication to combat breast cancer.
Posted on
Previous Article
« A systematic review of interventions to improve AET adherence in breast cancer survivors Next Article
Digital inhaler programme improves asthma control also in the long term, but not long-term adherence »
« A systematic review of interventions to improve AET adherence in breast cancer survivors Next Article
Digital inhaler programme improves asthma control also in the long term, but not long-term adherence »
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com