https://doi.org/10.55788/580043dc
No head-to-head trials have been conducted comparing injectable drugs, dimethyl fumarate, and teriflunomide, all approved for the first-line treatment of MS. Thus, Dr Clara López-Caneda (Hospital Alvaro Cunqueiro, Spain) and colleagues conducted a retrospective observational study to evaluate the relative effectiveness and persistence of these drugs in a real-world setting [1].
Between early 2015 and early 2024, the researchers included 400 patients who started a first-line MS treatment (132 patients with MS were prescribed injectable drugs, 130 dimethyl fumarate, and 138 teriflunomide). Clinical and radiological variables were compared. Efficacy was evaluated in terms of percentages of patients reaching NEDA-2 (i.e. absence of relapses and progression of disability) and NEDA-3 (i.e. NEDA-2 plus absence of new T2 lesions or Gd-enhancing lesions on brain MRI). Dropout was defined as DMT discontinuation for any reason for at least 6 months.
During the first year of treatment, 79.8% of the participants had NEDA-2 and 59.9% NEDA-3. Teriflunomide was associated with the most favourable outcome, with 87.0% of users reaching NEDA-2, compared with 77.6% on injectable drugs and 73.8% on dimethyl fumarate (P<0.05). The survival analysis yielded no differences between the treatments in reaching NEDA-2 (P=0.27) and NEDA-3 (P=0.95). Participants using injectable drugs had a higher dropout rate (62.12%) compared with dimethyl fumarate (43.08%) and teriflunomide (40.58%) (P<0.001). Treatment persistence was higher with dimethyl fumarate and lower with injectable drugs (P=0.01).
- López-Caneda C, et al. Persistence and effectiveness of moderate efficacy drugs in multiple sclerosis patients. Real world data. P382, ECTRIMS 2024, 18–20 September, Copenhagen, Denmark.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« BPROAD: Intensive or standard BP treatment strategy in type 2 diabetes? Next Article
SUMMIT: Tirzepatide reduces cardiovascular events in HFpEF plus obesity »
« BPROAD: Intensive or standard BP treatment strategy in type 2 diabetes? Next Article
SUMMIT: Tirzepatide reduces cardiovascular events in HFpEF plus obesity »
Table of Contents: ECTRIMS 2024
Featured articles
Diagnosis, Biomarkers, and Phenotypes
Revised McDonald criteria allow earlier and more precise MS diagnosis
Approaches to RIS and MS converge
AI versus clinicians: who diagnoses MS faster and better?
Blood markers predict MS progression
Gut microbiota modulate inflammation and cortical damage
Risk factors and importance of persistent PIRA
Vitamin D supplementation in progressive MS should be medically supervised
Treatment: Strategies
Encouraging real-world results of AHSCT to treat aggressive MS
CAR T-cell therapy in MS: in its infancy but highly anticipated
B cell-tailored dosing of ocrelizumab shows good results
First-line moderate-efficacy DMTs show similar efficacy
Treatment: Trials
Tolebrutinib slows disability worsening in relapsing MS
Frexalimab shows favourable safety and efficacy in OLE
Good safety of ozanimod over up to 8 years of treatment
Tolebrutinib slows disability in non-relapsing SPMS
High-dose simvastatin does not slow disability progression in SPMS
Comorbidity Risks and Pregnancy
High genetic burden for depression associated with MS disease activity
More comorbidity is associated with worse clinical outcomes in MS
Transfer of ocrelizumab into breastmilk is negligible
NMOSD/MOGAD
Ineffective response to EBV in MS not seen in similar diseases
Comparative effectiveness and safety of DMTs in NMOSD
Age, time, and treatment determine relapse risk in MOGAD
Related Articles
September 9, 2020
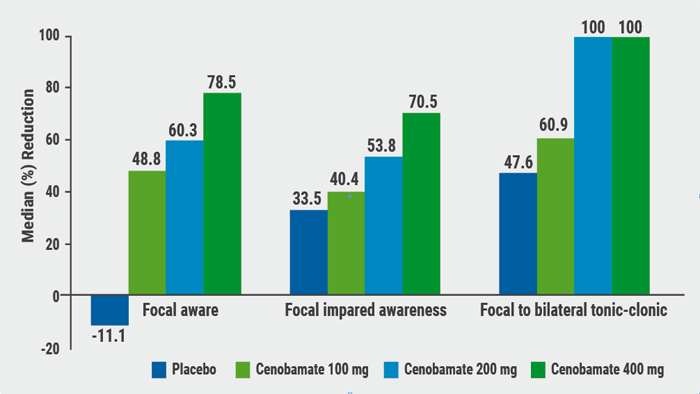
Cenobamate effective in focal epilepsy
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

