The aim of this retrospective cohort study was to investigate whether polysomnography-based sleep features are associated with the long-term risk of neurodegenerative disease [1]. Dr Abubaker Ibrahim (Medical University of Innsbruck, Austria) explained that the study cohort consisted of patients who were referred to the Sleep Disorders Unit of the Medical University Innsbruck between 2004 and 2007. The participants had to be ≥18 years of age, undergo polysomnography, and be free of neurodegeneration at baseline and during the first 5 years of follow-up. Of 1,454 assessed patients, 999 met these criteria (31.7% women; median age 54.9 years). Dr Ibrahim and colleagues wanted to know how many patients of this core group would be diagnosed with a neurodegenerative disease before the year 2022.
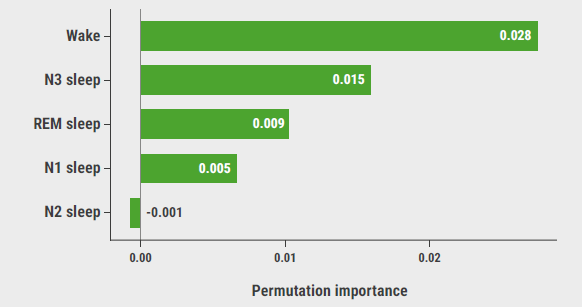
After a median of 12.8 years of follow-up, 75 patients developed a neurodegenerative disease; 924 did not. Dr Ibrahim showed that a 1% decrease in sleep efficiency, N3 sleep (i.e. deep sleep), or REM sleep was associated with a 1.9%, 6.5%, and 5.2% increased risk of incident neurodegeneration, respectively (HR 1.019, 1.065, and 1.052, respectively), after adjusting for demographic, sleep, and clinical covariates. A 1% decrease in waking within the SPT corresponded with a 2.2% reduced risk of incident neurodegenerative disease (HR 0.978). Assessed patients in the highest wake-in-SPT quartile (>18.6%) or the lowest REM sleep (<13.0%) or N3 sleep (0%) quartile had the shortest overall mean disease-free survival (14.9 years; 95% CI 14.6–15.3 years). Dr Ibrahim added that random Forest analysis showed that wake was the strongest predictor of neurodegeneration, followed by deep sleep and REM sleep (see Figure).
He concluded that altered sleep architecture can be used as a marker of neurodegenerative disease but perhaps also as a future target for neuroprotective strategies. “With this, I hope to have convinced you to have a good night's sleep and to convince your patients to do the same.”
Figure: Permutation importance of individual features derived from a random Forest analysis [1]
- Ibrahim A, et al. Sleep features and long-term incident neurodegenerative diseases: a polysomnographic study. EAN 2023 Annual Meeting, 1–4 July, Budapest, Hungary.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« Recent innovations in psoriasis Next Article
Nightmares during childhood linked to cognitive decline later in life »
« Recent innovations in psoriasis Next Article
Nightmares during childhood linked to cognitive decline later in life »
Table of Contents: EAN 2023
Featured articles
Letter from the Editor
Alzheimer’s disease and dementia: the road towards proactive and preventive care
Overarching Theme: Big Data
Contribution of genomics and genetics to personalised medicine
How big data can boost care for neurodegenerative disorders
COVID-19
Amantadine in early COVID-19 enhances recovery
SARS-CoV-2 vaccination in CIDP and MMN: more benefit than harm
Cerebrovascular Disease and Stroke
Intensive BP reduction associated with smaller haematoma
Cognition and Dementia
Towards cell biology of Alzheimer’s disease
Epilepsy
Minimising co-medication optimises cenobamate efficacy in drug-resistant epilepsy
Headache and Pain
GLP-1 agonists induce weight loss and alleviate headache in idiopathic intracranial hypertension
Cannabis-based medicine does not beat placebo in central neuropathic pain
80% of patients reverse from chronic to episodic migraine on anti-CGRP antibodies
Multiple Sclerosis
Which patients can initially be treated with platform DMT?
Retinal layer thickness predicts disability accumulation in early RMS
Withdrawing DMF in early pregnancy does not increase relapse risk in pregnant patients with MS
Immunosenescence and MS: relevance to immunopathogenesis and treatment
Sleep Disorders
Nightmares during childhood linked to cognitive decline later in life
Sleep changes contribute to the pathogenesis of neurodegenerative diseases
Miscellaneous
EAN guidelines on the management of ALS
What neurologists should know about bladder and sexual problems
Laughing gas abuse often leads to polyneuropathy, myelopathy, and encephalopathy
Related Articles
September 7, 2023
EAN guidelines on the management of ALS
September 7, 2023
What neurologists should know about bladder and sexual problems
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

