"The significant association of metabolic syndrome, diabetes and hypertension with cognitive dysfunction in individuals with schizophrenia indicates that clinicians need to keep the body in mind to improve physical outcomes and to not worsen already challenged cognitive functioning in this population," Dr. Christoph U. Correll of Northwell Health, in Glen Oaks, New York, told Reuters Health by email.
Dr. Correll and his colleagues examined data from 27 papers involving more than 10,000 patients. Information from 13 studies showed that patients with metabolic syndrome had significantly greater global cognitive deficits.
Data from eight studies indicated that this was also true of diabetes and five did so for hypertension. Among factors that led to deficits but did not reach significance were being overweight or obese, the researchers report in JAMA Psychiatry.
Analysis of cognitive subdomains showed that diabetes was significantly associated with poorer cognition in five of six domains. This was true of four of six domains for metabolic syndrome and four of five domains with available data for hypertension.
"Clinicians should preferentially choose antipsychotic treatments with the lowest possible cardiometabolic risk, promote healthy lifestyle behaviors and monitor weight and metabolic parameters as well as adherence to healthy lifestyle in all patients with schizophrenia aiming to optimize physical health, psychiatric and, possibly via beneficial effects on cognition, also functional outcomes," said Dr. Corrrell.
He added, "Prospective randomized trials are needed to investigate to what degree and in which patient populations targeted interventions aimed at restoring or maintaining healthy body weight and improved cardiometabolic status can significantly improve cognition and functional outcomes in individuals with schizophrenia."
Dr. Mark Olfson of New York State Psychiatric Institute, in New York City, told Reuters Health by email, "Cognitive impairment is common in adults with schizophrenia and may worsen as they age. This carefully performed meta-analysis confirms that metabolic syndrome, diabetes, and hypertension are related to global cognitive impairment in people with schizophrenia."
"These findings alert physicians to the need to monitor cognitive function particularly carefully in their patients with schizophrenia who have these cardiovascular risk factors," said Dr. Olfson, who was not involved in the study. "The results also underscore the importance of aggressively managing these conditions in people with schizophrenia through diet, exercise, appropriate pharmacological management, and selection of antipsychotic medications with fewer adverse metabolic effects."
SOURCE: https://bit.ly/38paIdv JAMA Psychiatry, online March 3, 2021.
By David Douglas
Posted on
Previous Article
« Neoadjuvant chemo for intrahepatic cholangiocarcinoma may prolong life Next Article
Cancer patients have higher readmission rates for heart attack, bleeding after PCI »
« Neoadjuvant chemo for intrahepatic cholangiocarcinoma may prolong life Next Article
Cancer patients have higher readmission rates for heart attack, bleeding after PCI »
Related Articles
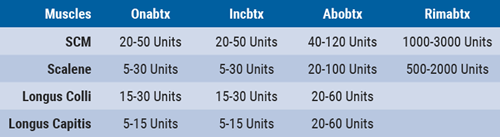
March 15, 2019
Anterocollis posture and deep cervical muscle injections
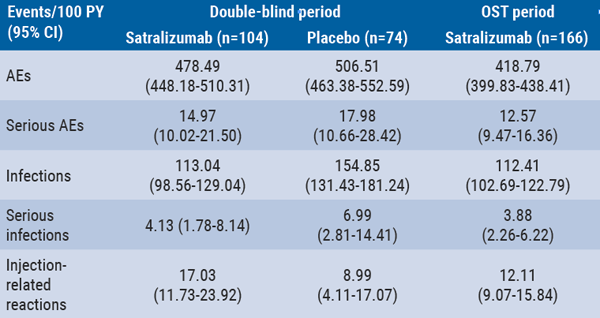
September 10, 2020
Long-term safety of satralizumab consistent with double-blind periods
July 30, 2021
Cannabis use disorders tied to increase in schizophrenia
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

