In subset analyses, however, patients with translocation t(11;14) and high BCL-2 expression appeared to reap the PFS benefit without increased mortality, researchers report in The Lancet Oncology.
"Addition of venetoclax to bortezomib and dexamethasone appears to improve the progression free survival and depth of response in relapsed myeloma," lead author Dr. Shaji K. Kumar of the Mayo Clinic in Rochester, Minnesota, the study's first author, told Reuters Health by email. "The benefit appears to be mostly in the t(11;14) subgroup of patients."
Between 15% and 20% of multiple myeloma patients have t(11;14), Dr. Kumar noted.
Venetoclax (VENCLEXTA, Abbvie and Genentech) has been approved by the U.S. Food and Drug Administration for treating chronic lymphocytic leukemia/small lymphocytic lymphoma and acute myeloid leukemia. The companies funded the trial and has financial ties to several authors, including Dr. Kumar.
In the BELLINI trial, 291 patients were randomly assigned 2:1 to 800 mg of venetoclax per day or placebo, along with bortezomib and dexamethasone. Patients received eight 21-day cycles of treatment followed by 35-day cycles until there was disease progression, intolerable toxicity or the patient withdrew.
Median follow-up was 18.7 months, and median progression-free survival (PFS) was 22.4 months with venetoclax and 11.5 months with placebo (hazard ratio, 0.63; P=0.01).
Treatment-emergent events included neutropenia, pneumonia, thrombocytopenia, anemia and diarrhea, and there were serious adverse events in 48% of the venetolax group and 50% of the placebo group.
Twenty-one percent of the patients on venetoclax died compared to 11% of those on placebo, with 7% and 1%, respectively, dying within 30 days of the last dose of study drug.
Eight fatal infections occurred with venetoclax, while there were none in the placebo group. Three deaths in the venetoclax group were considered treatment related versus none in the placebo group.
Among patients with either t(11;14) or high BCL2 gene expression or both, median PFS was not reached, while it was 9.9 months with placebo (hazard ratio, 0.21; P<0.0001). For patients without t(11;14) and low BCL2 expression, there was no significant difference in median PFS between those on venetoclax or placebo.
"In the patients with t(11;14), clinical trials are exploring how best to use this drug and which particular combinations with other myeloma drugs may have the maximum impact on outcomes," Dr. Kumar said.
Patients with myeloma cells expressing high levels of BCL2 appear to benefit from the drug regardless of whether they have t(11;14), he added, and efforts are underway to find a clinically useable biomarker test to identify them.
"The utility of venetoclax in earlier stages of disease such a smoldering multiple myeloma, as well as related disorders such as plasma cell leukemia and light chain amyloidosis, both of which have high proportion of patients with t(11;14) is being explored as well," he said.
"Given the findings from the BELLINI trial, it is important that patients on venetoclax treatment for multiple myeloma are followed very closely for risk of toxicities such as infections. Antibiotic prophylaxis is recommended for these patients. Physicians are encouraged to enroll these patients in clinical trials which will allow us to learn more about this drug," Dr. Kumar concluded.
"For the first time, we have precision medicine in myeloma," Dr. Irene Ghobrial of Dana Farber Cancer Institute and Harvard Medical School in Boston told Reuters Health in a telephone interview. Dr. Ghobrial wrote an editorial accompanying the study.
"Selecting the subgroup of patients who will benefit from therapy is important, and selecting the patients who won't benefit and may be harmed is also important," she added.
Dr. Ghobrial noted that t(11;14) is prevalent in Black Americans with multiple myeloma, so venetoclax may be especially beneficial for this population.
"Oncologists now will look at cytogenetics and fluorescence in situ hybridisation in multiple myeloma through a new lens, not only as prognostic markers, but also as biomarkers for therapeutic decisions," she writes in the editorial. "One hopes that this will translate into therapies for other genomic alterations in multiple myeloma, which, until now, were deemed untargetable."
By Anne Harding
SOURCE: https://bit.ly/3lf3Jbf and https://bit.ly/3kga4C0 The Lancet Oncology, online October 29, 2020.
Posted on
Previous Article
« Oasis Next Article
Children with Kawasaki disease need long-term surveillance for heart disease »
« Oasis Next Article
Children with Kawasaki disease need long-term surveillance for heart disease »
Related Articles
February 18, 2021
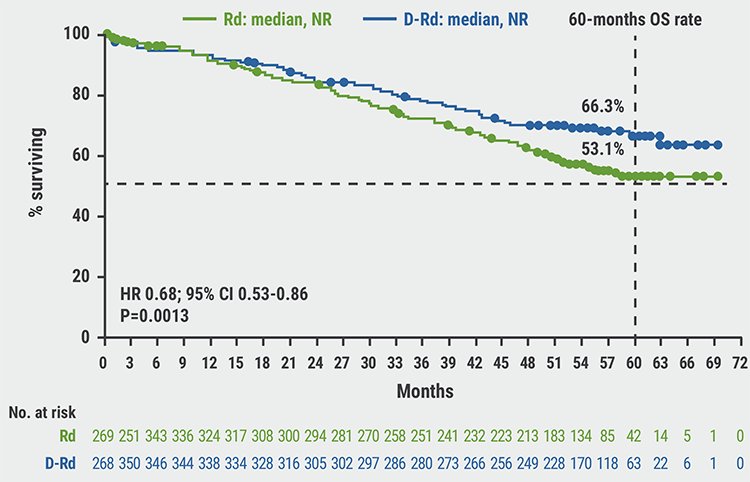
Survival of transplant-eligible newly diagnosed MM in FORTE trial
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

